Lupine Publishers | Open access Journal of Complimentary & Alternative Medicine
Keywords: Yoga; Therapy; Traumatic Brain Injury; Sleep; Mood; Depression; Anxiety; Adjustment
This project was funded by the Shepherd Center Research
Department located in Atlanta, GA.
To Know more Open Access Publishers Click on Lupine Publishers
Abstract
Sustaining a Traumatic Brain Injury (TBI) has a significant effect
on an individual’s physical and mental abilities. Residual
effects of TBI include sleep and mood disorders. Sleep disorders include
any disturbance in an individual’s quality of sleep and
daytime functioning. Mood disorders include depression, anxiety, and
adjustment to injury. Rehabilitation after TBI involves a range
of therapeutic services in which a holistic approach to therapy
addresses both the mind and the body. Yoga may be used to improve
functioning for individuals with TBI. The purpose of this convergent
mixed methods study was to examine the influence of yoga on
the sleep and mood in individuals with TBI. This research study involved
an eight-week yoga intervention at a large rehabilitation
hospital in the southern United States. Seven individuals who sustained a
TBI were recruited for the intervention. Sleep and mood
were assessed pre-, mid-, and post-intervention. Upon completion of the
intervention, participants and their caregivers took part
in focus groups to share their perceptions of changes in sleep and mood.
Data were analyzed and describe the influence of yoga on
individuals with TBI. Quantitative data revealed no statistical
significance, though percent change calculations of pre- and post-data
showed a substantial decrease in anxiety and an improvement in
adjustment to injury. Qualitative data were consistent with the
calculated percent change in addition to an emerging theme of social
support amongst individuals with TBI.
Keywords: Yoga; Therapy; Traumatic Brain Injury; Sleep; Mood; Depression; Anxiety; Adjustment
Introduction
A Traumatic Brain Injury (TBI) is defined as an acquired
injury that is the result of direct damage to the brain [1]. A TBI
can occur quickly and unexpectedly, but often has a long-term
effect on an individual’s physiological and neurological abilities
[2,3]. In the United States, approximately 1.7 million people per
year are admitted to the emergency room due to sustaining a TBI
[4], many of whom continue to live with residual effects [5]. The
residual effects of a TBI include, but are not limited to, trouble
sleeping, changes in mood, and difficulty adjusting to life after
injury [6,7]. Sleep disorders are defined as any consistent internal
disturbance in sleep [8]. Regarding people with TBI, poor sleep
quality is common [7] and has the potential to decrease emotional
and physical abilities, as well as slow the recovery process [9]. In
addition to the negative impacts from sustaining a TBI, individuals
are also susceptible to mood disorders as a residual effect of TBI.
Common behavioral impairments for people with TBI include
mood disorders, which can manifest as depression, anxiety, and
adjustment to injury [3,6]. Depression is a common secondary
factor for clinical conditions related to TBI [10]. Depression
is defined by the Diagnostic and Statistical Manual of Mental
Disorders (DSM-5) [8] as depressed mood or loss of pleasure in
life activities for more than two weeks, change from an individual’s
baseline mood, and compromised functioning. Generalized anxiety
is defined in the DSM-5 as extreme or unrealistic worry for the
majority of the days within six months [8]. Anxiety after TBI may
first be seen as a normal reaction to trauma, but individuals with TBI
appear to have an increased risk of developing generalized
anxiety in comparison to the general population [11]. Individuals
with TBI also experience an adjustment to life after injury [12].
Level of adjustment after sustaining a TBI can be observed through
the presence of depression, anxiety, fatigue, and irritability [13].
Due to the physical, cognitive, and emotional impacts of
sustaining a TBI, treatment for TBI needs to be approached
from a multidisciplinary perspective. As an emerging element of
physical rehabilitation, complementary integrative health (CIH)
interventions are health practices used in combination with
traditional medicine [14]. CIH includes a wide variety of healing
interventions that counteract illness or assist in increasing health
and wellbeing [15]. CIH interventions, such as yoga, can be used
as a holistic and complementary treatment to address the physical
and mental needs of individuals with TBI [16-17].
In the West, yoga focuses on three main practices: breathing
(pranayama), meditation (dhyana), and physical poses (asanas)
[18]. Yoga interventions have been utilized in several rehabilitation
settings [19-22], for the purpose of providing a complementary form
of therapy. Research on the perceptions of yoga, when integrated into
inpatient rehabilitation hospitals, shows patients’ rehabilitation
was enhanced by the use of yoga due to the added benefit yoga
provided, including self-management skills and assisting longterm
recovery [21,23]. Yoga for individuals with TBI is likely a
useful intervention due to the adaptability of yoga sequences, the
potential physical and cognitive benefits, and the research pointing
to the potential sleep and mood benefits [19-24]. While there
is limited research on yoga for TBI, one small, exploratory study
found that when yoga was administered 16 times over the course
of eight weeks, individuals with TBI expressed improvement in
physical, emotional, and mental domains [25]. In an analysis of the
influence of yoga on sleep for people with TBI through sleep-wake
diaries, a substantial improvement in sleep quality was found after
eight weeks of yoga treatment [19]. Following an adapted yoga
group intervention for individuals with TBI, participants expressed
favorable improvements in comfort with approaching balance and
relaxation, as well as an increased self-awareness that helped with
sleep [26]. There is limited research on yoga for individuals with a
TBI and yoga, thus there is need for further studies related to the
influence of yoga on sleep and mood in this population. Therefore,
the purpose of this study was to observe, analyze, and discuss the
influence of yoga on TBI related to their sleep and mood.
Methods
Design
This convergent mixed methods pilot study examined the
influence of yoga participation on sleep and mood among individuals
with TBI. Quantitative data was collected using a repeated measures
design, with pre-, mid-, and post-intervention assessments given.
Qualitative data was collected through two post-intervention focus
groups, consisting of one focus group with participants and one
with the participants’ caregivers. Prior to the start of this study,
approval through the Rehabilitation Hospital’s Institutional Review
Board (IRB) and the Clemson IRB were obtained.
Recruitment and Participants
Purposeful, criterion-based sampling was employed in this
study to decrease the variation of diagnosis amongst subjects [27].
Fifteen individuals who sustained a TBI and were prior patients at
a large rehabilitation hospital in the Southeastern United States,
that provides a continuum of care for individuals with TBI, were
contacted by the project coordinator. The project coordinator, a
Recreational Therapist at the rehabilitation hospital, screened all
individuals interested in the study using the Six-Item Screener
(SIS) to assess cognitive status in order to determine eligibility
for a program or intervention [28]. The SIS has been used as a
screener into yoga studies for individuals with TBI [20]. After
screening the individuals, the project coordinator reviewed the
inclusion and exclusion criteria with the individuals with TBI as
well as their caregivers, to determine if they met the inclusion and
exclusion criteria for the study. Inclusion criteria for persons with
TBI required that they:
I. Had diagnosis of moderate-to-severe TBI, verified by the
individual’s Glasgow Coma Scale score upon admission to the
rehabilitation hospital [29],
II. Were a fluent speaker of English, by self-report,
III. Were 18 years of age or older,
IV. Were able to move into different seated, standing,
and supine postures without assistance (based on self- and
caregiver-report),
V. Had a caregiver that was willing to assist with participant
transportation needs throughout the study, and
VI. Had sufficient cognitive status to participate, as
determined by a score of at least 4/6 on the Six-Item Screener.
The presence of any one of the following criteria resulted in
exclusion from the study:
A. were unable to attend 12 or more yoga classes during the
eight-week intervention,
B. had current drug or alcohol abuse, per self-report, and
C. enrollment in another intervention study that could
affect sleep or mood. Inclusion and exclusion criteria were also
established for caregivers of participants with TBI to ensure
they were able to fulfill the role of caregiver throughout the
study, although a caregiver was only required if the individual
with TBI needed assistance with daily tasks.
Inclusion criteria for the caregivers required that individuals:
a. were age 18 or older,
b. had no prior history of TBI,
c. were the self-identified caregiver of person with TBI,
d. were a fluent speaker of English, per self-report, as being
willing to transport participant to all yoga sessions related to
the study (as needed).
Exclusion criteria for caregivers of people with TBI were as
follows:
i. were unable to report on participant for whom they
provide care, and
ii. had current drug or alcohol abuse based on self-report.
All participants provided written informed consent prior to the
start of the study. Participants admitted to the study were given
a $25 incentive, funded by the rehabilitation hospital research
department for clinician research projects, upon completion of
the study.
Intervention
Yoga sessions were conducted in groups in a yoga room within
a large rehabilitation hospital in the Southeastern United States.
Sessions occurred twice a week for eight weeks, for a total of 16
yoga sessions. A recreational therapist who is a yoga teacher and
specializes in yoga for individuals with TBI taught all yoga sessions.
The sequences of yoga poses were designed based on the Love
Your Brain (LYB) Foundation yoga program, which is designed for
individuals with TBI [30]. The project coordinator of this study
adapted the LYB yoga sequences to fit this specific study group
[31], to focus on influencing sleep and mood. Changes to the LYB
protocol included increased time for meditation and a decrease
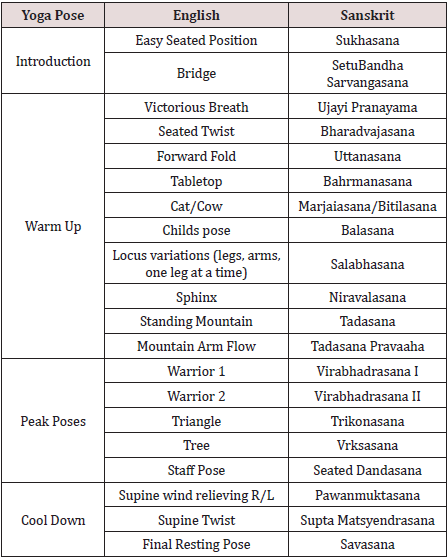
in poses accomplished on hands and knees. See Table 1 for yoga
sequence. Each yoga class was one hour long and included a
15-minute centering and focusing of the mind, 30 minutes of gentle
physical yoga postures in supine, prone, seated, and standing
positions, and 15 minutes of meditation and relaxation. The yoga
sessions remained at the same level of difficulty from start to finish,
in order to facilitate the transition from the rehabilitation setting to
the community setting by encouraging growth towards mastery of
the postures as opposed to growth in the number of postures.
Data Collection
Quantitative measures were chosen to focus on sleep and mood
for individuals with TBI. Qualitative data were collected through
post-intervention focus groups. The primary researcher conducted
all data collection.
Quantitative Measures
Sleep quality was measured using the Pittsburgh Sleep
Quality Index (PSQI), a self-report questionnaire used to assess
the quality of sleep over a one-month period [32]. The 24-items
inquire about sleep duration, sleep medication, sleep latency,
sleep quality, and how sleep effects an individual’s daytime activity
[33]. An individual may be diagnosed with poor sleep if he or she
has a global PSQI score of greater than five. The PSQI has been
used to screen for insomnia in individuals with TBI in post-acute
care [34]. The PSQI has a diagnostic sensitivity of 89.6%, and a
specificity of 86.5% when differentiating between individuals who
experience ‘poor’ or ‘good’ sleep [32]. Depression was measured
using the Patient Health Questionnaire-9 (PHQ-9). The PHQ-9 was
developed based on the DSM-V criteria of depression [8] and can be
self-administered [35]. The PHQ-9 is a nine-item depression scale
that measures level of depression over the past two weeks using
four-point likert responses, where 0=not at all, to 3=nearly every
day [36]. Once completed, the total score was summed to assess
level of overall depressive symptoms. The PHQ9 classifies level
of depression based on the sum of responses, with 0-4=minimal
depression, 5-9=mild depression, 10-14=moderate depression,
15-19=moderately severe depression, greater than 20=severe
depression [37], and a score greater than 12 is the cutoff for being
diagnosed with major depressive disorder [38]. The PHQ-9 was
also effectively used in a study on combat-related TBI [39].
Anxiety was measured using the Generalized Anxiety
Disorder-7 (GAD-7) survey. The GAD-7 is a seven-item anxiety
scale that measures level of anxiety of the past two weeks using
four-point likert responses, where 0=not at all, to 3=nearly every
day [40]. This self-report questionnaire has shown reliability and
validity [40,41] and can be used to analyze anxiety in the general
population [41]. The GAD-7 classifies level of anxiety based on the
sum of responses, with 0-4=minimal anxiety, 5-9=mild anxiety,
10-14=moderate anxiety, 15-21=severe anxiety, and a score greater than
10 is the cutoff for being diagnosed with generalized anxiety
disorder [40]. The GAD-7 was validated in primary care facilities
[36] but has also been used to measure anxiety in a study on
sleep and psychological conditions after sustaining TBI [42] and
used to measure anxiety related to mild TBI related to combat
[39]. Adjustment was analyzed using Part B of the Mayo-Portland
Adaptability Inventory (MPAI-4). The MPAI-4 has four parts, each
of which address a different aspect of adjusting to injury. Part B was
selected due to the specific focus on adjustment to injury related
to an individual’s mood (irritation, aggression, pain, depression,
anxiety, fatigue, social interaction, self-awareness, and sensitivity to
symptoms). The rating scale ranges from 0-4, from 0=no problem
to 4=severe problem that interferes with activities more than 75%
of the time [43]. A sum score of 0-7= mild limitations, 8-15=mild
to moderate limitations, 16-24=moderate to severe difficulties, and
>25=severe limitations with a score of less than seven indicating a
good outcome [44]. This scale was designed to assist in the clinical
evaluation of participant adjustment during the post-acute (post
hospital) period following an acquired brain injury [13]. This
scale has been used in multiple rehabilitation settings, including
post-acute rehabilitation, comprehensive day treatment, and
community-based rehabilitation [45-47].
Qualitative Data Collection. As a convergent mixed methods
study, this intervention was best examined through multiple
forms of data, addressing research questions in a general and
broad quantitative fashion, as well as providing a narrative and
explanatory qualitative aspect [48]. The participant focus group
focused on the participant’s experience in the yoga intervention,
giving an account of their experience, any change they noticed
in sleep, depression, anxiety, or adjustment to injury, and any
additional comments they had about the influence of yoga over
the past eight-weeks. The caregiver focus group facilitator asked
similar questions and focused on the caregiver’s observation of
participant behavior over the past eight-weeks. These focus groups
were held in the private yoga room at the rehabilitation hospital
and recorded using two audio recorders.
Data Analysis
Quantitative Analysis
Descriptive statistics were used to describe demographics,
which included age, gender, marital status, race, work status,
education, time (in years) since injury, and cause of injury.
Nonparametric analysis was indicated because of the low sample
size; thus, the Friedman Test was used to compare mean ratings
of each assessment, using the Statistical Package for the Social
Sciences (SPSS) software version 24. Comparisons were made
between the group mean Pittsburgh Sleep Quality Index (PSQI)
scores, depression scores (PHQ-9), anxiety scores (GAD-7), and
adjustment scores (MPAI-4, Part B) from pre, mid, and postintervention
assessments. To further examine the quantitative
results using the means from each assessment, percent change was
calculated using the following formula:
Pre-intervention = [(post-intervention value–pre-intervention
value)/pre-intervention value] x 100%.
Qualitative Analysis
The qualitative focus groups were transcribed verbatim to
increase descriptive validity [49], and participants and caregivers
were assigned a subject number to ensure confidentiality.
The project coordinator observed the focus groups to ensure
interpretive validity [49], reporting that the project coordinator
and primary researcher shared the same perceptions of the focus
group discussion. After initial transcription, the primary researcher
reviewed the qualitative data for themes, and categorized the
responses based on their connection to sleep, depression, anxiety,
and adjustment to injury. The project coordinator and an additional
researcher reviewed the transcripts from the focus groups before
and after analysis to check for consistency and establish interrater
reliability [50]. In accordance with Creswell and Creswell’s
sequential process of qualitative analysis [50], focus group
transcriptions were organized and read thoroughly by the primary
researcher. Coding was deductive, to identify patterns within the
data relevant to predetermined outcomes (i.e., sleep and mood),
and to determine the existence of any emergent codes.
Mixing Quantitative and Qualitative Data
Qualitative and quantitative data were collected and analyzed
separately [50]. After individual data analysis, quantitative and
qualitative data were compared to discover converging or differing
results [48].
Results
Overall, 15 people were contacted and invited to participate
in eight weeks of yoga. Ultimately, seven people passed the SIS,
met the inclusion criteria, and committed to the study, while eight
declined despite having passed the SIS, citing scheduling conflicts,
distance from home, lack of interest, and inability to commit to
eight sequential weeks. Six people completed the study, five of
whom had caregivers, while one person dropped out of the study
1.5 weeks prior to completion due to travel conflicts. Of the six
participants who completed the study, four (67%) were female, and
the average age was 31, with the ages ranging from 21-43 years
old. The majority of participants were White (66%), and most were
single (83%). Half of participants had a graduate degree, although
50% were unable to work. The average time since injury was 4.67
years. On average, participants attended 14 of the 16 sessions,
with an attendance rate of 89% based on total number of sessions
offered. See Table 2 for additional participant demographics. In
the following sections, both quantitative data and qualitative data
are provided by outcome, as the intent of this convergent mixed
methods design was to compare converging or differing results
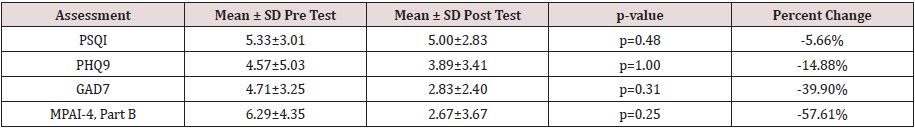
[48]. See Table 3 for the mean pre and posttest, p-value, and percent
change.
Sleep
The Friedman Test revealed that quality of sleep did not differ
significantly when comparing pre-, mid-, and post-intervention
PSQI scores (X2=1.46; p=0.48). The percent change from the preand
post-intervention scores yielded a result of -5.7% change,
indicating a minor decrease in reported issues related to sleep. The
qualitative data on sleep was convergent with the quantitative data,
supporting that there was no significant change in sleep quality for
most participants. Most caregivers and participants commented
on an improvement in sleep since the individual sustained the
injury, but most did not identify further improvement as a result
of the yoga intervention. However, one caregiver believes yoga
has enabled her loved one to have deeper rest while sleeping. The
caregiver stated that her loved one has “deeper sleep, she sleeps
longer in the morning, has trouble to wake up, and she dreams.
And she remembers her dreams!” In addition, one participant
commented on her ability to sleep, saying sleeping in the past year
“I would hear any little noise, it’d just bother me and wake me. So,
sleep with earplugs, I slept with earplugs and an eye mask for light.
Now I’m much better and I don’t need earplugs or a mask.”
Depression
The quantitative and qualitative data showed converging results
regarding depression, as neither form of data collection identified
substantial changes following the yoga intervention. The Friedman
Test showed insignificant results regarding pre-, mid-, and post-
PHQ-9 data (X2=0, p=1.00), while the percent change from the preto
post-intervention assessment was -14.9%, indicating a slight
decrease in depression. Depression was briefly highlighted in the
participant focus group, as one individual stated “I’ve never seen
myself as depressed,” and later said “I don’t think I’m depressed
but again, the doctors have attributed my past tiredness and
sluggishness to depression, and they say that now that I am active,
it helps that aspect.”
Anxiety
No significant difference in anxiety was found using the
Friedman Test (X2=2.33, p=0.31). However, the percent change from
pre- to post-test was -39.9%, representing a substantial decrease
in anxiety after the yoga intervention. Complementing the percent
change calculation, both caregivers and participants provided
meaningful comments related to a decrease in anxiety during
focus groups. Caregivers stated that yoga was “calming,” “relaxing,”
and “increased the awareness” of their loved ones. Participants
shared similar thoughts, using the words “calming” and “relaxing”
throughout their discussion of their yoga experience. One caregiver
stated: What my daughter seems to get out of it more than anything
is the mindfulness and the meditation and just calming her down.
Because we go at a high pace, and so this is a good way for her to just
relax and help her brain get better. In addition, another caregiver
said “she’s maybe more relaxed I would say. Less anxious.” Later
on, this same caregiver explained, that yoga “sets her back and
somehow it’s relaxing in order to let other things than the panic
in her mind.” Participant responses aligned with the caregiver
perspectives, as participants commented, “yoga has always relaxed
me,” and “it helps me loosen up.” Another participant expressed
her appreciation of yoga, saying: It’s perfect how the practice slows
down, repeats, and just focuses on just a healthy mind. So, whereas
out in the world, we’re supposed to go, go, go. Here we can just slow
down, be in our minds, be present, and just be.
Adjustment
Though quantitative data regarding adjustment to injury
produced non-significant findings based on the Friedman Test
(X2=2.80, p=0.25), the calculated percent change from the preto
post-intervention MPAI-4 Part B assessment was -57.6%,
indicating a considerable decrease in issues related to adjustment
to injury. In addition, the qualitative data showed an improvement
in adjustment. Qualitative data showed an increased interest in
activity and self-esteem, as well as a decrease in irritability from
the perspective of both the caregivers and the participants. When
asked about a change in amount of activity for individuals with TBI,
one caregiver said, “he’s interested in doing more than just this.”
When asked the same question, a participant stated, “I do want to
do more activities outside of the house.” Moreover, one participant
explained, “I do have more endurance of being able to take on more
activities throughout the course of the day.” Caregivers emphasized
an increase in self-esteem following the yoga intervention. One
caregiver commented on the relationship between improvement in
self-esteem, and the eight weeks of yoga, saying:
Self-esteem I think is a big problem. I mean, a huge problem.
But um, maybe for the past two months she, I think she’s more
aware and more in acceptance. So, it seems like the self-esteem is
less of a problem.
While another caregiver explained that her husband is
considering taking initiative on a project that she relates to
an increase in self-esteem. Concerning irritability, a caregiver
stated her son is “definitely getting more pleasant to be with,”
and a participant said “yoga, being mindful, the whole practice of
presence and really being intentional and present with what you’re
doing has positively affected the way I approach anything.” Social
Support in the TBI Community. Though not included in the purpose
of this study, appreciation of the community that formed as a result
of the yoga intervention was evident as a theme throughout the
caregiver and participant focus groups. In the profound words of
a caregiver, yoga has provided “a place [for the participants] to
be injured.” Caregivers expressed “it’s just nice to be with people
who are maybe dealing with the same things,” “they need groups
to socialize, to exchange because they’re very lonely,” and yoga has
“been wonderful for him because the rest of the time he is in the
home alone.” In line with caregiver responses, a participant stated
that yoga helps in “having community support others who know
your situation, experience, having gone through the same things.”
One participant expressed an appreciation of the ability to share
experiences, saying “it’s better to have friends that you can meet
actually, all of you, and to know that they’re doing the same thing
that you have to.” The community developed through yoga is unique
due to the emphasis on rest and relaxation, which one caregiver
highlighted by saying “yoga allows them to have time to think…
we’re not the ones that are gonna settle down with them like ‘ah,
let’s rest’…we don’t have the time and probably not the patience
either.”
Discussion
The primary purpose of this pilot study was to examine the
influence of yoga on individuals TBI related sleep quality and mood
after eight weeks of bi-weekly yoga. There was not a substantial
change in sleep based on the PSQI. The data in this study differ
from previous research that found yoga to improve sleep [19,51].
Though sleep disorders are common for individuals with TBI [7],
the majority of this study population did not express complaints
with sleep prior to or after the yoga intervention, resulting in
little to no change in quantitative and qualitative results related
to sleep. Considered to be a residual effect of sustaining TBI [52],
depression was expected to be present in this study population.
The pre-intervention average depression score from the PHQ9 was
4.57, (just beneath the mild depression score of 5-10), showing
that participants did not initially experience significant depression
symptoms. Depression was not significantly impacted by the yoga
intervention, though the percent change showed a slight reduction
in depressive symptoms, consistent with previous research
claiming yoga yielded decreased reports of depression [53].
The findings of this study support previous work that yoga has
the potential to decrease symptoms of anxiety [7,16,54]. Though
quantitative measures yielded insignificant results, the percent
change showed a substantial decrease in symptoms of anxiety. The
qualitative data also demonstrated a reduction in anxiety, which
participants identified was due to the emphasis on the calming
and relaxing effect of yoga. Furthermore, a study by Verma et al.
identified a decrease in anxiety continued beyond the yoga session
was supported by caregiver and participant perspective shared
during the focus groups [7].
Although not statistically significant, adjustment to injury did
substantially improve, as indicated in the percent change calculation
and the qualitative data. In congruence with the claim that yoga
contributes to overall adjustment for individuals with TBI [55], this
yoga intervention contributed to a decrease in irritability, and an
increase of interest in activities. In addition, focus group discussions
showed considerable improvement of self-esteem and selfawareness,
supporting previous work that demonstrated the ability
to improve emotional awareness through yoga after sustaining TBI
[56]. The yoga intervention focused on awareness of the body and
the mind by encouraging participants to bring awareness to specific
body parts at time and acknowledge certain emotions that may
come up. The focus on awareness throughout each yoga session
likely contributed to the comments on increased self-esteem and
awareness, consistent with the study results on the impact of an
8-week yoga program for individuals with TBI that indicated an
improvement in self-perception [57]. A theme of social support
through the yoga intervention became apparent through the focus
group discussions. In a study on social support for individuals with
TBI, Stålnacke [58] found reports of low-quality social support due
to lack of social interaction. Consistent with results from other yoga
studies [59-62], caregivers and participants described the yoga sessions
as beneficial due to the sense of camaraderie with people
who have similar life changes due to sustaining TBI. Caregivers
expressed the need for their loved ones to be with other people due
to their loss of friends since sustaining TBI. Discussions during both
caregiver and participant focus groups indicated an appreciation of
the shared experience yoga provides. Participants in an inpatient
rehabilitation setting benefited from the social interaction provided
by yoga [21] supporting the theme of social support that emerged
from this pilot study.
Implications for Further Research and Practice
The diverging results from quantitative measures and
qualitative interpretations specific to the influence of yoga on
sleep and mood indicate a need for further investigation. In order
to expand this study, future research should consider including
only those with current complaints related to sleep and mood
and involve a larger sample size. Future studies may also consider
the use of a yoga sequence that becomes progressively more
challenging, as the content of the yoga intervention used in this
study maintained the same level of difficulty from start to finish.
A progression of poses may produce more substantial results, as
challenging activities are more likely to produce change [63]. Yoga
is a valuable therapy that can be implemented in a rehabilitation
setting [21,23,64]. Attendance was high due to the location of the
yoga intervention, since the rehabilitation hospital was a familiar
place to all participants. Participants and caregivers also stated that
they would like to see yoga included in TBI rehabilitation and they
also identified the desire for the yoga intervention to continue and
be offered individuals in outpatient programs. The qualitative data
supported the value of yoga within a TBI rehabilitation setting as it
can decrease anxiety, improve adjustment to injury, and promote
social support within the TBI community.
Limitations
Due to the nature of research, this pilot study has limitations.
This study took place in one rehabilitation hospital in the
southeast and cannot be generalized to all yoga programs within
a rehabilitation hospital. Second, while we aimed to observe
the influence of yoga on ten people, only six people remained
committed to the study from start to finish, resulting in a small
sample size, where it is difficult to determine statistically significant
changes in outcomes. More clearly stating attendance requirements
when recruiting participants may increase commitment to the
study. This study was not blind to the primary researcher or the
participants, as the primary researcher was in direct contact with
the participants, and the participants were informed of the purpose
of the study when recruited for the study. Due to the pilot nature
of this study, no control group was observed in comparison with
the individuals receiving the yoga intervention. By adding a control
group, researchers may be able to further understand the influence
of yoga versus other environmental and social influences. Finally,
the yoga sessions were not designed to build on themselves, but
rather involved the same primary moves with variations according
to the yoga instructor’s preference. A yoga sequence that becomes
progressively more challenging may yield stronger results.
Acknowledgement
For more Complimentary & Alternative Medicine Open Access Journal articles Please Click
To Know more Open Access Publishers Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublisher
Follow on Twitter : https://twitter.com/lupine_online


No comments:
Post a Comment
Note: only a member of this blog may post a comment.