Lupine Publishers | LOJ Medical Sciences
Introduction
The incidence of medical mistakes in primary care is not rare and the probability of faults producing grave detriment is great. Medical negligence is a ‘tort’, or ‘civil wrong’. It is a ‘wrong’ resulting from a doctor’s carelessness. Simply put, negligence means failing to do something that should have been done as defined by current medical practice or doing something that a physician with a duty to care for the patient should not have done. Whereas about one percent of hospital admissions result in an adversative event due to negligence, faults are probably much more common, because these studies detect only errors that led to assessable adversative events occurring soon after the mistakes. Moreover, though after heart disease and cancer, medical mistake is the 3rd important reason of death in the USA, maybe the real problem in medical faults is not bad persons in health care; rather it is that good individuals are working in corrupt systems. Poor communiqué , blurred lines of power of doctors, nurses, and other care providers, incoherent recording systems, differences in healthcare provider teaching and practice , failure to recognize the frequency and significance of medical mistakes, overestimation of insufficient data, sleep deficiency and night shifts, doctor’s depression, fatigue, and burnout , unfamiliar settings, diverse patients, and time pressures have been accounted as vital causes of medical error. In the following article, some proven neurologic cases, which have been diagnosed in the beginning by at least one neurologist as conversion disorder and referred to psychiatric facilities, have been described. This article tries to give the reader an awareness regarding the aforesaid dilemma, in the ground of psychological medicine.
Background
Clinical forensic medicine is a term that has become widely used only in recent decades, though the phrase has been in use at least since 1951. The practitioners of clinical forensic medicine have been given many different names thru the years, but the term forensic physician has become more widely accepted. In broad terms, a forensic pathologist generally does not deal with living individuals, and a forensic physician generally does not deal with the deceased. However, worldwide there are doctors who are involved in both the clinical and the pathological aspects of forensic medicine. There are many zones where both clinical and pathological aspects of forensic medicine overlap, and this is reflected in the history and development of the specialty as a whole and its current practice [1]. The current data indicates that medical mistakes kill yearly around 180 000 individuals in hospitals and medical faults may be the fifth foremost reason of death in the United States of America. If these implications are exact, the present health care system can be accounted, as well, as a community health threat [1], and the existing scheme of medical negligence or misconduct does a poor job as regards the wellbeing of patients. Societal and economic powers are changing the structure of health care from the individual doctor to a union of health care specialists, categorized by liable medical groups [2]. On the other hand, enterprise accountability, joined with medical slip communication and corrective platforms, delivers the lawful agenda essential for the ‘patient-centered’ practice of medicine in current situation [3]. The word ‘error’ in medicine is utilized as a term for approximately all of the complications hurting the patients. Also, medical mistakes are often designated as human faults in healthcare [4]. Whether this label is ‘human error’ or ‘medical error’, one description used for it in medicine pronounces that it happens when a healthcare worker selects an unfortunate mode of care or incorrectly performs a proper technique of care. Anyway, a medical fault is an avoidable adversative consequence of care, whether or not it is hurtful or manifest to the patient. This might contain an erroneous or imperfect management or diagnosis of a behavior, syndrome, disease, infection, damage, or other illness [2].
According to a national survey in United Kingdom, each year, medical errors costing in excess of two billion ponds [5]. Another study has found that drug mistakes are among the most common medical errors, hurting as a minimum 1.5 million individuals each year. Likewise, medical faults, globally, affect at least one in ten patients [6]. According to the findings of a new study, after heart disease and cancer, medical mistake is the 3rd important reason of death in the USA. It deserves to be mentioned that The Institute of Medicine (IOM) released “To Err is Human,” in 2000, which stated that the real problem in medical faults is not bad persons in health care-it is that good individuals are working in corrupt systems that should be prepared safer [6]. Moreover, poor communiqué and blurred lines of power of doctors, nurses, and other care providers are among the causative issues [6]. Incoherent recording systems in a hospital may cause disjointed systems in which frequent handoffs of patients ends in lack of harmonization and mistakes [6]. Differences in healthcare provider teaching & practice and failure to recognize the frequency and significance of medical mistakes as well intensify the threat [7,8]. Then again, the supposed ‘July effect’ happens when firsthand residents come to training hospitals and instigating an upsurge in medication mistakes [9,10]. Jerome Groopman, author of ‘How Doctors Think’, has assumed that these are ‘cognitive pitfalls’, or biases which can cloud our judgment. For instance, a physician may overestimate the first data run into his head, influencing his decision. Another drawback is where stereotypical presumptions may skew intelligence [11].
Sleep deficiency has also been mentioned as a causal reason in medical mistakes [11]. According to a study, being awake for above twenty four hours could cause medical interns to ‘double’ or ‘triple’ the number of avoidable medical faults, involving those that had caused harm or decease [11]. Similarly, night shifts are connected with poorer surgeon performance through laparoscopic surgeries [11]. Doctor’s risk factors consist of depression, fatigue, and burnout [12]. Issues related to the clinical setting, too, include unfamiliar settings, diverse patients, and time pressures [11]. All of the following case examples, which have been chosen in this regard, have been diagnosed primarily and unreasonably, by at least one neurologist as conversion disorder and referred to psychiatric facilities. This article tries to give the reader awareness about the aforesaid dilemma, in the ground of psychological medicine. Names, dates and locations have been omitted totally to keep the confidentiality of the cases.
Case 1
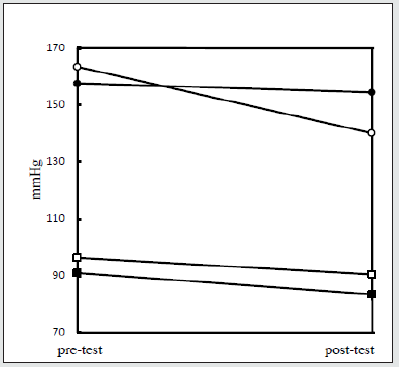
A 42 years old male driver had been referred by his general physician to a neurological clinic after observing some tremors in the upper limbs of the patient. The patient had been visited due to sleep problems and nervousness. According to the patient, his problems had been started a few weeks after his divorce from his wife, which had been occurred one year earlier due to various financial and family problems. The care of children also had been transported to him. While the primary prescription of fluoxetine, 20- 40 milligram per day, could only mitigate some of the psychological symptoms like anxiety and dysphoria, the aforesaid tremor got worse, which had not respond to 30 milligram propranolol per day, too. So, he had been referred to a neurologist for further analysis. After primary checkup and based on the personal and family history, since no specific finding was evident at clinical exam, he had been prescribed a series of drugs, in accompany with the aforesaid fluoxetine, like Primidone, 500 milligram per day and Trihexyphenidyl 6 milligram per day, with the primary diagnosis of essential familial tremor, which could be aggravated, too, by means of psychological stresses and maybe small amounts of antipsychotis (Perphenazine, 4-8 milligram per day which had been prescribed by the GP due to his aggressiveness). After another six months, due to intensification of tremor that had interfered with some of his daily activities, and also his anxiousness he had been referred to a consultant psychiatrist. In the initial examination, in addition to a relatively fluctuating tremor, between fine and course, depending on the situation of the limbs, some mild rigidity as well was palpable in the proximal muscles of the upper limb, without any evident cogwheel or clasp-knife rigidity. Due to lack of obvious concern in him regarding his earlier divorce or similar worries, absence of strong or insistent relationship between tremor and psychosocial stresses, unexplained mild rigidity of the proximal muscles of the upper limbs in spite of discontinuation of antipsychotic, and no satisfactory response to the abovementioned medications, so he was referred again for another neurologic evaluation. This time, due to low serum ceruloplasmin level (17 mg/dl), low serum copper (55 microgram/dl), and increased urinary copper excretion (150 microgramm Cu in 24 h) , presence of copper deposition in Descemet’s membrane (Kayser-Fleischer rings) in slit-lamp examination, and slightly enlarged lateral and third ventricles, widened cerebral and cerebellar sulci, and hypodensity of posterior parts of lenticular nuclei in CT Scan , plus bilateral, symmetrical signal hyperintensities in the Basal ganglia, Midbrain, Pons, and Thalamus in T2-weighted MRI, the diagnosis of Wilson’s disease (Hepatolenticular Degeneration) had been suggested for him and thus transferred to a neurologic clinic for further investigation and management.
Case 2
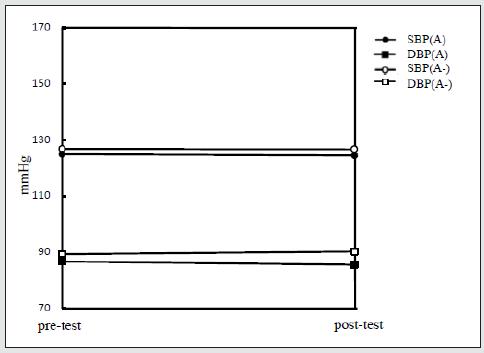
A 38 years old man had been hospitalized in the psychiatric ward due to aggressiveness, suspiciousness, disturbed sleep and some movement problems. When he was 18-year-old, he had been diagnosed as a case of bipolar I disorder due to similar profile of symptoms, except than movement problems, which had been started since two years ago. During the last two decades a number of neuroleptics, mainly first-generation antipsychotics, mood stabilizers like lithium and valproate, and benzodiazepines had been prescribed for him. One year ago he was hospitalized again in another psychiatric hospital for his increasing movement problems, which had been assigned to his antipsychotic medications, and had been treated by dopaminergic drugs like Levodopa – Carbidopa (Sinemet) (750-1000 milligram per day), Amantadine (200 milligram per day), and also Trihexyphenydil (6 milligram per day). The aforesaid problem had been diagnosed as medication induced movement disorder (pseudo-parkinsonism) by a consultant neurologist. But there was lack of effectiveness and worsening of the problem. After the recent admission and disregard to the past and present psychiatric history of anxiety, depression, impulsiveness, dis-inhibition, suspiciousness or paranoid delusions, in the clinical examination a mild-moderate fluctuating rigidity and tremor in the upper and lower limbs was evident, which had made clumsiness and unsteady gait, respectively. Also, there were some problems regarding swallowing solid foods and talking fluently. Also, a fixed stare with a smiling expression and drooling was evident. So, another neurologic consultation had been requested by his psychiatrist; this time also, the antipsychotic induced movement disorder had been confirmed, once more, by the second consultant neurologist, who, moreover, proposed tardive Parkinsonism as a probable differential diagnosis. Due to lack of effectiveness of the aforesaid treatments, in spite of discontinuation of prescribed antipsychotic (Quetiapine 75 milligram per day), Electroconvulsive therapy (ECT) was started, which stopped after five sessions, due to existence of mild fever and lack of significant effect. Nonetheless, due to refractoriness of the movement symptoms against the recommended treatments, their fluctuating course and persistence in spite of discontinuation of neuroleptics, atypical emergence and persistence of the primary psychopathology, and a long gap (18 years) between the first prescription of neuroleptics and subsequent emergence of movement symptoms, an additional neurologic consultation had been requested for the patient. This time, a suspicious serum ceruloplasmin level (23 mg/dl), low serum copper (76 microgram/ dl), and increased urinary copper excretion (153 microgram Cu in 24 h) had been found. MRI scan, too, had showed decreased signal intensity (hypodensity) in the Striatum and superior Colliculi and increased signal intensity in the Midbrain Tegmentum (except for red nucleus) and in the lateral Substantia Nigra (reticular zone). So, diagnosis of Wilson’s disease (Hepatolenticular Degeneration) had been suggested for him and transferred to a neurologic facility for further investigation and management.
Case 3
A forty seven years old father with a at least five percent weight loss in the last year, in spite or normal appetite and sleep, had been examined by an internist, but the primary laboratory examinations and clinical checkups, including thyroid analyses and computed tomographic scan (CTS), had not proved any specific medical diagnosis. So due to slight restlessness, increasing feeling of tiredness and loss of energy in comparison with before, nervousness, irritability and decrease in attentiveness had been referred to a psychiatrist for analysis regarding psychological problems. In the mental state examination, and in addition to the abovementioned complaints, a slight forgetfulness, disturbance in concentration, negative thoughts, minor disturbance of conduct, history of enuresis during childhood, and a past history of mixed anxiety and depressive disorder after his father’s death, were as well detected, which in sum concluded to a diagnosis of mild to moderate major depressive disorder for the present episode of illness. But the primary medicinal management with fluoxetine, 20- 60 mg per day in a two months period, was not effective. So after a consultation with an associate neurologist and based on newly detected anomia, verbal perseveration, small time disorientation, trivial mood swings, score of 17 in Mini Metal State Examination (MMSE), and history of some head traumas with decrease of consciousness in the past, the diagnosis turned to pre-senile dementia and the aforesaid psychiatric complaints had been classified as secondary symptoms due to that. So, treatment with Rivastigmine, 3-6 mg per day, in addition to fluoxetine, started. But ineffective outcomes after another two months and the progressive course of the ailment resulted in an additional consultation with another teammate neurologist. After a new clinical inspection and detection of trivial fasciculation in upper limbs, muscle atrophy and weakness in upper extremities in Electromyogram (EMG), and atrophy of the frontal and/or temporal lobes in Magnetic Resonance Imaging (MRI), the diagnosis turned to Fronto-Temporal Degeneration (FTD) with motor neuron disease (FTD/MND) , and the patient transferred to a neurologic facility .
Case 4
A 23 years old man had been hospitalized due to restlessness, aggressiveness, decreased sleep, increased libido, delusion of grandeur, and obsession. The incessant and fluctuating course of the problems had been started from around four years ago with a series of psychiatric hospitalizations and managements. He had been diagnosed as a case of bipolar mood disorder, schizophrenia, and schizoaffective, or schizo-phreniform disorder during different periods and treated with a series of mood stabilizers, like lithium and sodium valproate, and also antipsychotics, and benzodiazepines. But during the past few years, he was never completely symptomfree, in spite of relative compliance with the prescriptions. During his recent admission, a dystonic reaction, as well, appeared in the neck which was resistant against anticholinergic drug (Biperidene, 6 milligram per day) and decreasing the dosage of antipsychotic (Risperidone). So, he had been referred to a consultant neurologist, who diagnosed medication induced movement disorder, in addition to the formerly diagnosed primary psychiatric disorder, and added Trihexyphenidyl (6-12 milligram per day, instead of Biperidene) and Amantadine (100-200 milligram per day) to the previous prescriptions. After two weeks of current treatment, due to persistence of dystonic reaction, and also lack of suitable response of psychiatric symptoms to prescribed medications, particularly their fluctuating course, firm delusion of grandeur and impaired judgment in spite of the apparently intellectual insight (IV/V) and normal cognitive & sensorium parameters, another neurologic consultation had been asked for the patient. So, based on the extensive bilateral and symmetrical calcifications in the basal ganglia, thalamus, and cerebellum, in CT Scan and MRI, and ruling out Hyperparathyroidism and Pseudo-Hypoparathyroidism , as major differential diagnostic considerations in the evaluation for treatable causes of diffuse subcortical calcifications , the primary diagnosis changed to Idiopathic Basal Ganglia Calcification or Bilateral Striato-Pallido-Dentate Calcification (Fahr’s disease) and the patient transferred to a neurologic facility for further investigation.
Discussion
The Diagnostic and Statistical Manual of Mental Disorders (DSM) (American Psychiatric Association 1994, 2000) contains current standard psychiatric diagnostic nomenclature used for clinical diagnosis, treatment, and research. The development and adoption of DSM diagnoses have been accompanied by a great deal of controversy [12]. Nevertheless, DSM diagnoses are generally accepted and relied on in clinical and research venues, as well as many other venues for which the nomenclature was not intended, including insurance companies, managed care companies, and the courts. The more significant question raised by the acceptance and reliance of the legal system on DSM is whether DSM diagnoses provide an adequate understanding of psychological states for forensic purposes. Legal determinations, whether civil or criminal, typically revolve around issues of impairment [12]. A DSM diagnostic category is not directly relevant to such determinations. Diagnosis and impairment are not equivalent. No diagnosis carries specific information regarding level of impairment or information about whether an impairment associated with that diagnosis is relevant to the legal issue under examination by the court. The use of categorical DSM diagnosis in litigation may result in the examiner missing the most important aspect of the forensic evaluation: the assessment of impairment or legally relevant behavior [12].
Medical negligence is a ‘tort’, or ‘civil wrong’. It is a ‘wrong’ resulting from a doctor’s carelessness. Simply put, negligence means failing to do something that should have been done as defined by current medical practice or doing something that a physician with a duty to care for the patient should not have done [13]. Medical error has been defined as the failure of a planned action to be completed as intended (an error of execution), an unintended act (either of omission or commission) or one that does not achieve its intended outcome, a deviation from the process of care that may or may not cause harm to the patient, or the use of a wrong plan to achieve an aim (an error of planning). Also, patient maltreatment from medical mistake can occur at the individual or system level. Todays, the categorization of faults is getting bigger to better classify avoidable causes and happenings [14]. While about one percent of hospital admissions result in an adversative event due to negligence, faults are probably much more common, because these studies detect only errors that led to assessable adversative events occurring soon after the mistakes [14]. Though independent review of doctors’ management policies proposes that decision-making could be enhanced in fourteen percent of admissions, many of the profits would have late expressions [14]. Even this amount may be an underestimate [14]. Medical faults are connected with inexpert doctors and nurses, innovative techniques, complex or urgent care, and extremes of age. Unfortunate communiqué, unreadable handwriting, inappropriate documentation, insufficient nurse-topatient proportions, and alike named drugs are similarly identified to contribute to the problem [15].
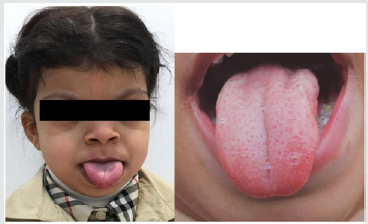
The same problem exists as well as regards the mental illnesses. For example, patients with ‘dissociative identity disorder’ typically have past psychiatric histories that encompass three or more separate mental disorders and prior treatment failures [16]. The skepticism of some physicians about the legitimacy of ‘dissociative identity disorder’ may similarly increase its misdiagnosis [16]. As an additional example, female sexual dysfunction occasionally used to be identified as female hysteria. Or else, food allergies have been repeatedly misdiagnosed as anxiety disorder . Likewise, investigations have found that bipolar mood disorder has often been misdiagnosed as major depressive disorder [16]. While the misdiagnosis of schizophrenia is as well a common problem, there may be long delays before getting an accurate diagnosis [16]. For the same reason, the DSM- Five field trials have included ‘test-retest reliability’, which involved different clinicians doing independent assessments of the same patient - a new method for studding diagnostic trustworthiness [16]. Anyway, back to medical illnesses, according to a meta-analysis the five most usually misdiagnosed diseases are cardiovascular disease, myocardial infarction, infection, neoplasm and pulmonary emboli [17]. On the other hand, while doctor acquaintance with this data is variable [18], faults can have an intensely negative emotional influence on the physicians who commit them [19]. As has been stated before, some researchers believe that adversative consequences from medical mistakes generally do not occur owing to isolated faults and essentially reflect system difficulties [20]. Such an idea is frequently referred to as the ‘Swiss Cheese Model’. This is the impression that there are strata of safeguard for patient and clinicians to avoid errors from happening. So, even if a physician or nurse makes an unimportant fault, this is exposed before it really jeopardizes patient safety (for example, pharmacologist checks the medications and corrects the slip). Such mechanisms include: Systematic safety methods, practical modifications, training programs, and persistent specialized progress courses [21]. On the other hand, medical and, particularly, neurological illnesses happen repeatedly among patients with conversion disorders. What is naturally seen in these co-morbid medical or neurological disorders is an expansion of symptoms arising from the original biological lesion. Somatization disorders, anxiety disorders and depressive disorders are particularly famous for their relationship with conversion disorder. Meanwhile, studies of patients admitted to a psychiatric hospital for conversion disorder, later, disclose that 25% to 50% have a clinically noteworthy mood disorder or schizophrenia. Similarly, personality disorders, too, often accompany conversion disorder, principally the passive-dependent type (9 to 40 percent of cases) and the histrionic type (in 5 to 2 1 percent of cases). The identification of conversion disorder necessitates that clinicians find an obligatory and important link between the source of the neurological symptoms and psychological dynamics, though the symptoms should not result from the factitious disorder or malingering. No doubt, one of the major difficulties in identifying conversion disorder is the problem of absolutely exclusion a medical ailment. Parallel nonpsychiatric medical disorders are common in hospitalized patients with conversion disorder, and evidence of a present or preceding neurological illness or a systemic disease affecting the brain has been reported in 18% to 64 % of such patients. As has been stated before, an estimated 25 to 50 percent of patients classified as having conversion disorder eventually receive diagnoses of non-psychiatric medical or neurological disorders that could have produced their prior symptoms. Accordingly, a systematic neurological and medical workup is necessary in all cases. Neurological disorders [e.g., dementia and other degenerative diseases], basal ganglia disease and brain tumors should be considered in the differential diagnosis. For example, weakness may be confused with multiple sclerosis, poly-myositis, acquired myopathies, or myasthenia gravis. Similarly, optic neuritis can be misdiagnosed as conversion disorder blindness. Other illnesses that may cause perplexing symptoms are Creutzfeldt-Jakob disease, Guillain-Barre syndrome, early neurological manifestations of acquired immunodeficiency syndrome (AIDS) and periodic paralysis. While conversion disorder symptoms occur in schizophrenia, depressive illnesses, and anxiety disorders, these other disorders are related with their specific distinct symptoms that sooner or later make differential diagnosis probable. In both factitious disorder and malingering, the symptoms are under conscious, voluntary control [13]. Because somatoform disorders are positioned at the crossroad between somatic and mental sicknesses, their differential diagnosis tends to be relatively all-encompassing.
However, there are numerous characteristics of these illnesses that can assist the differential diagnosis. For example, the presentation of rather ambiguous and multiple physical symptoms originating from several organ systems should usually propose a somatoform disorder instead of a somatic ailment. As the number of somatic symptoms rises [irrespective of whether they are pathologically clarified or inexplicable], so does the probability that those persons will meet criteria for a psychiatric illness, not a medical sickness. The following features can help in deciding whether idiopathic somatic symptoms may have a psychiatric etiology: 1- The symptoms co-exist with important psychiatric illnesses such as depression or panic disorder, 2- The symptoms strictly occur after traumatic events, 3- The symptoms lead to psychological “gratification” or “secondary gain”, 4- The symptoms characterize anticipated personality traits (coping mechanism)], 5- The symptoms become inflexible, join a conglomerate of other symptoms, and express such approaches as overuse of medical facilities and disappointment with medical care. The more of the abovementioned features that are present, the more likely it is that symptoms can be categorized as somatoform symptoms. In general, differential diagnosis from other psychiatric disorders is also difficult because many of the somatic symptoms may be related to a psychiatric disorder such as depression (e.g., pain symptoms), anxiety (e.g. cardiorespiratory and gastrointestinal symptoms), or even psychotic disorders (somatic delusions). Nevertheless, the existence of a great level of idiopathic somatic symptoms has to be considered even if they appear in the context of what is viewed as another primary disorder such as depression or anxiety because they probably affect symptom strictness, management outcome and level of incapacity [22].
Anyhow, careful medical examination, based on adequate clinical skills and knowledge, is necessary for diagnosis or ruling out of medical problems. Enhanced educational curriculums in medical schools, improvement of skills and knowledge of medical students in the field of ‘somatic symptom disorder’ and consultation-liaison psychiatry, guideline modifications, continuous post-graduation education and system modifications possibly will help to decline the percentage of medical errors [23]. Though no one has considered the total expenses of misdiagnosis of medical illnesses, it is clear that, if the mistake in diagnosis results in the deceases of patients, then the cost is tremendously high. Consequently, it may be wise that the diagnosis of conversion disorder not be seen as an absolute choice between biological vs. psychological symptomatology. However, if the diagnosis of conversion disorder is assumed, the clinician is recommended to prudently monitor current symptomatology to guarantee discovery of a biological pathology.
Conclusion
The incidence of medical mistakes in primary care is not rare and the probability of faults producing grave detriment is great, of which most could be taken as avoidable or fixable, if management could be started almost immediately or at least not too late. Sufficient attention to detailed process of development of patient’s symptoms, their intensity, duration, priority and fluctuation, and, moreover, vigilant medical checkup and thorough documentation of findings are helpful issues for further lessening of medical and diagnostic faults. So, a rigorous work and all-inclusive approach is compulsory for improvement of patient’s safety in primary care clinics. This may contain enhanced educational core curriculums in medical colleges, with an improved emphasis on psychological medicine, strengthening the validity and reliability of available diagnostic criteria, constant post-graduate training, and organizational amendments or revisions based on periodic re-evaluations. Supplementary studies respecting the prevalence, etiology, cultural or societal issues, student, faculty or facility related aspects, curriculum efficiency, and objective self-monitoring mechanisms certainly will help to reduce the problem.
Read More About Lupine Publishers Journal of Medical Sciences Click on the Below Link:
https://lupine-publishers-medical-sciences.blogspot.com/