Lupine Publishers | Journal of Otolaryngology
Abstract
Objective: FB (foreign bodies) in ear, nose and throat
are often encountered by otolaryngologists in their daily practice and
is
commonly seen in both children and adults. Depending upon the
type and location of FB, it may have serious impact on individual’s
health if instant appropriate action is not taken. That’s why,
there’s frequent visits to ED (emergency department) on having FB in
ear and aerodigestive tracts. The objective of this study was
to evaluate the nature, common sites, modes of presentation, modes of
management of FB, age and gender distribution.
Materials and Methods: A retrospective hospital-based study was done in Universal College of Medical Sciences, Bhairahawa,
Rupandehi, Nepal from March 2014 to September 2017. The information was obtained from hospital record books.
Results: Out of 483 total patients, 287 (59.42%) were
male and 196 (40.57%) were female. Most of them were less than 10
years old. Of the 483 patients, 202 (41.82%) had FB in the
ear, 132 (27.32%) in the nose and 149 (30.84%) in the throat. Living FB
were found in 54 (26.73%) patients out of 202 in the ear, 10
(7.57%) patients out of 132 in the nose and none in the throat. Of the
total patients, 97 (20.08%) required general anesthesia (GA)
to remove FBs and the rest 427 (88.4%) patients were dealt with or
without local anesthesia. Most of the FBs were removed
promptly on presentation otherwise within 24 hours of presentation in
the
hospital.
Conclusion: FB in ENT were found more commonly in the
children and the commonest site was ear. Timely presentation,
prompt diagnosis and needful management in a center with
otolaryngology practice reduces the morbidity and mortality. Most
of the FB in ENT can be removed in outpatient department (OPD)
or emergency room (ER) with or without local anesthesia (LA).
Keywords: Ear; Nose; Throat; Foreign Bodies; Local Anesthesia
Introduction
A foreign body (FB) is any object or substance that is not
derived from the individual’s own body part and can cause harm by its
mere presence if prompt medical care is not provided [1,2]. They may be
found in Ear, Nose and Throat. They are very common in
otorhinolaryngological clinical practice. It can be introduced
spontaneously or accidentally by both children and adults. However,
children are common victims as they have habit of inserting nearby
objects in their nose, ear or mouth, imitation and also other
contributing factors are like boredom, playing, mental retardation,
insanity, and attention deficit hyperactivity disorder, along with
availability of the objects and absence of watchful caregivers.
Consequently, it may cause minor irritation to life threatening problem.
A proper technique, good light, appropriate instrument, a co-operative
or fully restrained patient and a gentle approach by the related doctor
or health worker are required for the removal of FB. One should have a
clear diagnosis before making attempts to remove the FB so as to lessen
the morbidity [3,4]. FB may be classified as animate (living) and
inanimate (nonliving). The inanimate FB can again be classified as
vegetative (organic) and non-vegetative (inorganic) FB, and hygroscopic
(hydrophilic) and non-hygroscopic (hydrophobic) [1,2]. The objective of
this study was to evaluate the nature, common sites, modes of
presentation, modes of management of FB, age and gender distribution.
Materials and Methods
A retrospective study was conducted in the Department of ENT –
Head and Neck Surgery, Universal College of Medical Sciences, from
March 2014 to September 2017. The data were obtained from the hospital
record books. Otoscopy and anterior rhinoscopy were performed to
diagnose FB of the ear and nose respectively. Instruments such as Jobson
Horne probe, FB hook, Tilley’s forceps, and crocodile forceps were used
in FB removal from the nose and ear. Syringing and suctioning were also
done for FB ear removal. Plain X-ray of the neck was done in patients
with a history of FB ingestion. Flexible nasopharyngo laryngoscopy (NPL)
and flexible upper gastrointestinal (UGI) endoscopy were done in cases
where the FB was not visible in X-ray to rule out presence of a FB or to
determine its site of impaction and in selected cases UGI endoscopy was
used for FB removal too. It was followed by removal of the FB from the
oropharynx/hypopharynx and esophagus with direct laryngoscopy or rigid
esophagoscopy, respectively under general anesthesia (GA). FB struck in
the oropharynx or parts of hypopharynx were confirmed with the help of
Lack’s tongue depressor and head light or indirect laryngoscopy and
removed with the Tilley’s forceps under local anesthesia (LA) in the OPD
with patient co-operation.
Results
There were 483 patients recorded, out of which 287 (59.42%)
were male and 196 (40.57%) were female with male to female ratio 1.46:1.
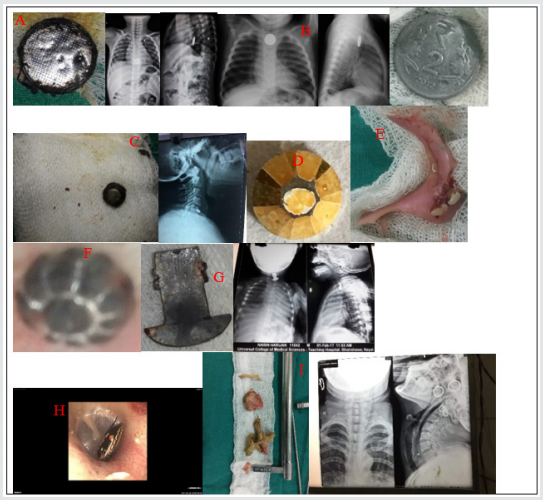
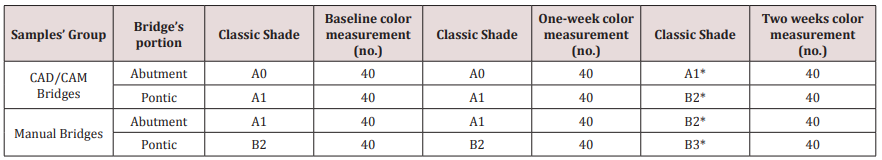
The number of FB (Table 1 & Figure 1) in ear was 202 (41.82%), 132
(27.32%) in nose and 149 (30.82%) in the throat. Out of 202 FB in ear,
54 (26.73%) was animate and 148 (73.26%) inanimate. Out of 132 nasal FB,
10 (7.57%) was animate and 122 (92.42%) was inanimate. The FB
encountered in throat was entirely of inanimate nature.
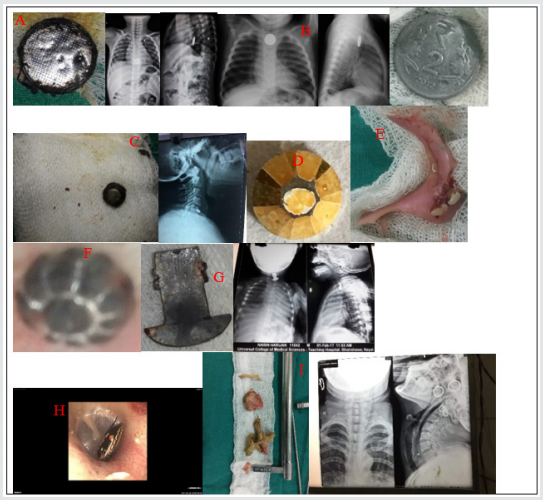
Figure 1. Few examples of ENT foreign bodies.
A) FB toy battery in esophagus and removed with rigid esophagoscope,
B) FB
coin in esophagus,
C) FB button battery in esophagus,
D) FB bead removed from ear,
E) FB denture,
F) FB bead removed from
nose,
G) FB metal hook in esophagus,
H) FB insect in ear and
I) FB chicken bone with meat bolus in esophagus.
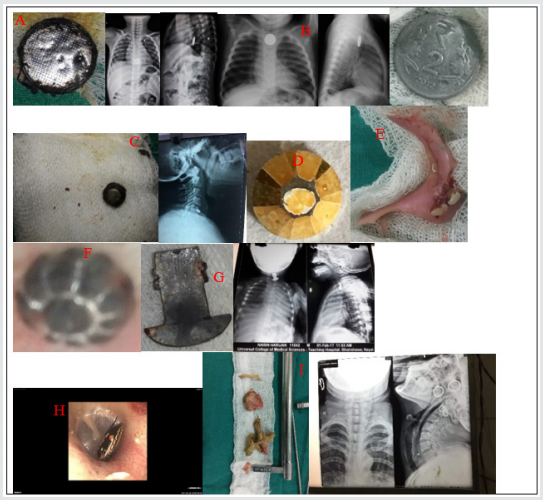
FB in Ear
Total of 202 patients were recorded with FBs in the ear. The
most common type of FB in the ear was grain seed 25.74% (52) followed by
FB bead 19.8% (40). Fifty-four (26.73%) patients had animate (living)
FBs. These were mostly insects in the form of maggots, cockroach,
grasshopper, butterfly, housefly and ticks. Hundred and forty-eight
(73.26%) patients had inanimate (nonliving) FBs. Out of 148 patients,
fifty-two (35.13%) had hygroscopic FBs in the form grain seed in the
form of bean, pea, wheat, paddy and gram as shown in Table 1. The rest
ninety-six (64.86%) patients had non-hygroscopic FBs in the form of
bead, cotton pledget, pebble, eraser, paper, button batteries, plastic
ball and vegetable twig or thorn. Majority of cases were seen in 0-10
years age group i.e. 72% (147). The most common site of FB lodgement was
found to be the external auditory canal. Most of these FBs were removed
in the OPD or in the ER with or without local anesthesia (LA). In 4
children, the FB were found impacted in the deeper part of EAC (3 button
batteries and 1 plastic ball) and had to remove under GA via post-aural
approach.
FB in the Nose
Hundred and thirty-two (27.32%) had FB lodgement in the nose.
The most common was grain seed 40 (Out of it, only 10 (7.57%) patients
had living FBs i.e., 9 had maggots and 1 had leech. The rest 122
(92.42%) patients had nonliving FBs as shown in Table 1. Forty FB
(30.3%) were of hygroscopic nature in the form of grain seed and the
rest sixty nine percent being non-hygroscopic as in Table 1. Of the
total number of 132 patients 122 patients (92.42%) were children and the
rest 10 (7.57%) patients were adults with animate type of FBs. Hundred
and five (86.06%) of the children presented with history of FB insertion
nose by their caretakers, while in 17 (12.87%) children neither the
patients nor the caretakers were certain of FB insertion. Unknowingly,
they were treated as a case of sinusitis due to complaints of nasal
blockage, headache and unilateral fetid discharge by the pediatricians
and primary care physicians, which was later, referred to our center and
revealed to be forgotten FB. Sometimes, even one has to depend on
imaging like x-rays /CT scans to rule out the FBs where the patients are
unable to recall the events. Otherwise, most of the times the typical
history provides clue for clinching the diagnosis. Most of the FB were
removed in the ER and OPD with or without LA and only 3 cases (2.27%)
required removal under GA i.e. 2 cases of beads and 1 case of grain seed
which on manipulation went posteriorly and also patient being
uncooperative.
Foreign Bodies in the Throat
A total of 149 patients presented with the complaint of
ingestion of FB. The most common type of FB was coin of one rupee, 2, 5
and 10 rupees and the common site of the impaction was cricopharyngeal
junction in all the 50 patients (33.55%). The sites of other types of FB
impaction were oral cavity, oropharynx, hypopharynx, thoracic esophagus
and lower gastro-esophageal sphincter region. All the ingested FB were
inanimate, with 84 (56.37%) being organic and 65 (43.62%) being
inorganic. Organic FBs were meat bolus and bone (fish, chicken, mutton,
and buffalo meat) and one of plum seed. The inorganic FBs included
button battery, thorn, denture, coin, and metallic objects as shown in
Table 1. Age less than 10 years old were the most common group with FB
coin. FBs fish bone and vegetable twig/thorn lodged in oral cavity and
oropharynx were removed under LA. Out of 40 FB coin, 10 were dislodged
spontaneously via gastrointestinal route, 5 FB meat bolus and 7 FB
chicken bone were removed by flexible endoscopy and the rest of the FBs
were removed under GA without postoperative complications.
Table 1. Different types of Foreign bodies (FB) in ENT.
Discussion
In our study, we’ve found higher incidence of FB in children
less than 10 years old in 66.04% (319) patients. This is consistent with
study by Iseh and Yahya [5], Ogunleye AOA and Sogebi R [6], Ahmad M, et
al. [7]. This may be consequent of children’s exploring habit and
lodging objects into the natural orifices of body, accidentally or
intentionally. We found 59.42% of patients to be male and 40.5% to be
female with male: female ratio 1.46:1. The male: female ratio was shown
to be 1:1.05 by Gregogri et al. [8] whereas it was 1:1.26 in the study
of Ogunleye AO et al. [9] and 1.35:1 by Agrawal S, Ranjit A study [10].
This suggests male are more susceptible than female to foreign body
insertion in the orifices. In this study we observed ears were the most
common site of lodgement of foreign bodies (41.82%) followed by throat
(27.32%) and nose (27.32%). Parajuli R [11] and Shrestha I, et al. [4]
also found in their study ears as the most common site for impaction of
foreign bodies followed by throat and nose. The most common foreign
body in the ear and nose was the variety of grain seeds like bean, pea,
paddy, wheat, gram, maize and foreign body coin was highest in throat.
Removal methods, most commonly used for ear, nose and throat FBs were
similar to those presented by Parajuli R [11], in order of preference
the alligator forceps, Jobson Horne probe, foreign body hook, Tilley’s
forceps and ear syringing. No patient required endoscopy or indirect
laryngoscopy to remove oropharyngeal FB. The need for general anesthesia
to remove FB varies in literature, with percentages varying from 8.6%
to 30% [12]. There were no complications reported post FB removal.
Conclusion
FB in ENT are common in both pediatric and adult population.
Comparatively the children are seen to be more vulnerable to have ENT FB
lodgement. Significant complications may arise if FB in ENT are not
taken care of immediately and skillful removal is must. Thus, proper
care and watch must be provided by care takers or the family members in
order to prevent the encounter of such objects, especially in pediatric
group.
Read More Lupine
Publishers blogger Articles: https://lupinepublishers.blogspot.com