Lupine Publishers | Advancements in Cardiovascular Research
Abstract
Hypertrophic cardiomyopathy (HCM) is the most common cardiac disease
affecting the cardiac muscle. It can manifest in
different forms with or without left ventricular outflow obstruction,
with or without right ventricle involvement. Forms with
biventricular hypertrophy seem to have poor prognosis. In our case, we
describe a young patient with sarcomeric biventricular
hypertrophic cardiomyopathy (MYH7 mutation), the poor prognosis of this
form and strategies options adopted after failure of
medical treatment. It is not always easy the management of hypertrophic
cardiomiopathy, after medical treatment failure, especially
in children. In some cases, heart transplantation is the only one
therapeutic option.
Keywords: Hypertrophic Cardiomiopathy; Right Ventricular Hypertrophy; Heart Transplantation
Introduction
Hypertrophic cardiomiopathy (HCM) is the most common
cardiac disease affecting the cardiac muscle and is characterized
by heterogeneous genetic, morphological, functional, and clinical
features. It is also one of the main causes of sudden cardiac
death (SDC) in the young. Left ventricular hypertrophy with left
ventricular outflow obstruction (LVOTO) is the most characteristic
feature of HCM. There are also variant of HCM without LVOTO, with
apical hypertrophy, with medio-ventricular obstruction and with
right ventricular hypertrophy. The treatment and the prognosis of
HCM seem to be variable on the basis of different forms, the age
at presentation, sarcomeric gene mutations or rare phenocopies.
Heart transplantation (HT) is the only therapeutic option for
selected patients with HCM and refractory heart failure. In effect
ESC guidelines recommend heart transplantation in eligible
patients who have an LVEF < 50% and NYHA functional Class
III–IV symptoms despite optimal medical therapy or intractable
ventricular arrhythmia (II a); in eligible patients with normal LVEF
(50%) and severe drug refractory symptoms (NYHA functional
Class III–IV) caused by diastolic dysfunction (II b)[1].
Right ventricular hypertrophy (SRVH) is a relatively rare
subtype of HCM. The anatomic, genetic, clinical, and prognostic
characteristics of patients with SRVH and the clinical relevance
of these characteristics have not been described widely in the
literature [2,3]. MYBPC3 gene mutations have previously been
described in two patients with RV hypertrophy. In a recent study,
90% of HCM patients with SRVH were found to possess relevant
sarcomere protein mutations and variations in the MYH7 (Myosin
heavy chain 7) and TTN genes, followed by variations in MYBPC3.
Always in this study 73% of HCM patients with SRVH and multiple
sarcomere gene mutations had poor prognosis. 7 In addiction MYH7
mutations can cause hypertrophic cardiomyopathy or skeletal
myopathies with or without cardiac involvement, on the basis of
the side of mutation. In our case, we describe the poor prognosis
and treatment strategies of a young patient with biventricular
hypertrophic cardiomyopathy and MYH7 mutation.
Case Report
A 12-year-old young woman with familiarity for hypertrophic
cardiomyopathy (mother and mother’s twin with biventricular
hypertrophic cardiomiopathy and MYH7 mutation) was hospitalized
in our hospital for dyspnea after mild-moderate efforts and
reduced functional capacity (NYHA Class II). Mother and aunt of the
patient were asymptomatic with good functional capacity. Patient had the same genetic mutation of mother and aunt (p.Asn696Ser
heterozygosis MYH7) but with increased and poor phenotypic
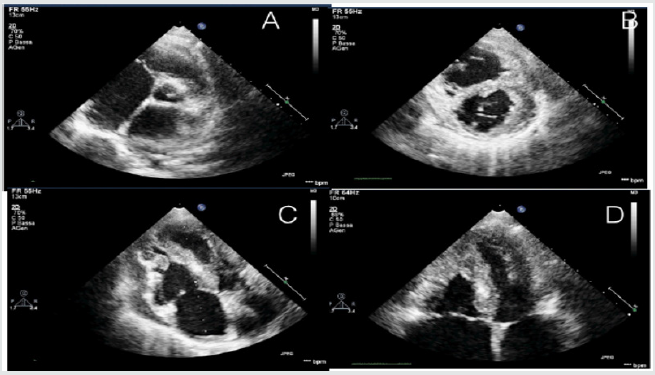
expression [4]. Echocardiography and cardiac magnetic resonance
were performed showing a hypertrophic cardiomyopathy with
right ventricular involvement. Precisely, cardiovascular imaging
showed left ventricle asymmetric hypertrophy especially at the
level of anterior and inferior wall (basal and mild anterior wall
=14 mm, z score= 3,5; antero-lateral basal wall = 12 mm, z score
2,78; mild inferior wall = 14 mm and apical inferior wall = 12 mm)
with normal ejection fraction (FE = 62% at CMR) and moderate
diastolic dysfunction (panel B and D). In addiction wall thickness
of right ventricle outflow and basal-mild free wall were increased
(= 13 mm) with apical obstruction and development of maximum
gradient of 10 mmHg (PANEL A and C) [5,6] (Figure 1).
The function of right ventricle was at inferior limits (FE = 51%
at CMR, TAPSE = 16 mm at echocardiography). Thus the patient had
an interesting right ventricle involvement and moderate diastolic
dysfunction of left ventricle. She had not arrhythmia at ECG-Holter
but she had reduced functional capacity. also demonstrated at stress
test. Stress test was suspended at 6 min (Bruce Protocol) after
pre-syncopal symptoms: lack of adaptation of the blood pressure
to the effort was observed. In addition, from several months she
had pre-syncopal episodes at the peak of the effort. ECG showed
left ventricular hypertrophy and biatrial enlargement. Pro BNP was
increased = 5841 pg/ml. Considering clinical situation, we decided
to start medical treatment with betablockers (bisoprolol) but the
patient didn’t tolerate medical treatment. Thus, we decided to start
low dose of captopril without improvement of symptomatology.
Also, treatment with diuretic was not tolerate by patient [7,8].
Therefore, considering symptom refractory to medical therapy, the
poor prognosis and the impossibility to optimize medical treatment,
we decided to plan cardiac transplantation, the only option possible
at this moment.
Thus right catheterization was performed and patient was
inserted in heart transplantation list. ICD implantation was not
considered in the absence of ventricular arrhythmia and other
factors. Discussion: hypertrophic cardiomyopathy associated with
MYH7 mutation and right ventricle involvement seems to have
poor prognosis, especially if right ventricle hypertrophy is severe
[9]. In effect the young patient had a greater right ventricular
hypertrophy compared than mother and aunt. In these cases, after
medical treatment failure, heart transplantation seems to be the
only strategy to improve symptomatology and quality of the life of
the patient. Especially in pediatric population, it is not always easy
the management of hypertrophic cardiomiopathy after medical
treatment failure and heart transplantation seems to be the only
one therapeutic option. Other study are needed to study some
variants of HCM with right ventricle hypertrophy, their treatment
and prognosis.
Read More Lupine Publishers Journal of Cardiology & Clinical Research Articles :
Read More Lupine Publishers blogger Articles : https://lupinepublishers.blogspot.com
| https://lupine-publishers-cardiovascular.blogspot.com/ |

No comments:
Post a Comment
Note: only a member of this blog may post a comment.