Lupine Publishers | Advancements in Cardiovascular Research


Read More Lupine Publishers blogger Articles : https://lupinepublishers.blogspot.com
Abstract
TakotSubo Cardio Myopathy (TSCM) is a reversible form of
cardiomyopathy characterized by transient left ventricular (LV) systolic
dysfunction. Clinically often mimics acute myocardial infarction (AMI)
with chest pain or breathlessness with electrocardiographic,
cardiac marker(s) and LV wall motion abnormalities. In a third of
patients, significant emotional or physical stress precedes the
presentation. Often, these patients have normal epicardial coronaries or
non-flow obstructive coronary disease. In most patients,
LV function shows complete recovery within weeks with favorable
outcomes. We report a unique case of TSCM following sudden
emotional stress with typical transient apical ballooning; nevertheless,
with severe co-existent triple vessel coronary artery disease
and complete recovery of cardiac function on medical management.
Keywords: Tako-Tsubo Cardiomyopathy; Apical Ballooning; Coronary Artery Disease
Case Presentation
73 year old hypertensive female admitted with sudden onset
intermittent chest pains and shortness of breath (< 24 hours after
the death of her granddaughters in a road traffic accident). There
were no other significant past medical history of note and she never
smoked. On arrival, she was tachycardic (heart rate 102) in sinus
rhythm, normotensive and clinical examination was unremarkable.
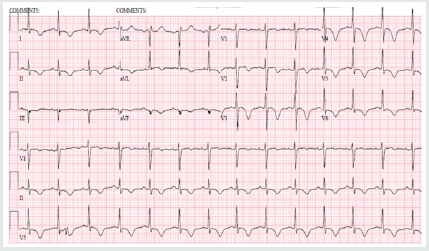
Her initial ECG (Figure 1) demonstrated sinus tachycardia with
deep T wave inversions in both precordial and limb leads. Her
bloods revealed high sensitivity Troponin-T of 395ng/L [normal
reference range <15ng/L]. Her bedside echocardiogram revealed
typical pattern of “apical ballooning” with severe hypokinesis in the
anterior, lateral, septal and inferior walls of the left ventricle, sparing
the basal walls. Her left ventricular systolic function was moderately
impaired with an ejection fraction (EF) of 40% (Figure 2). Both her
clinical presentation and echocardiographic appearances were
highly suggestive of “Takotsubo Cardiomyopathy”. Nevertheless,
she was conventionally treated for presumed “Non-ST elevation
myocardial infarction (NSTEMI)” at the initial stages [1].
Figure 1: ECG on admission showing sinus rhythm with deep T-wave inversions in both precordial and limb leads.
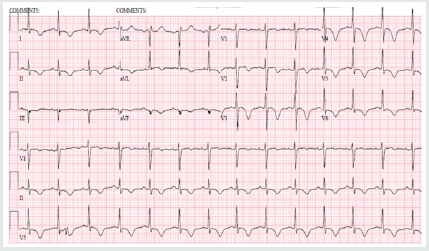
Figure 2: 2-D Transthoracic echocardiogram (apical view) revealing typical apical ballooning with akinetic apical wall and
preserved basal contraction of left ventricle.

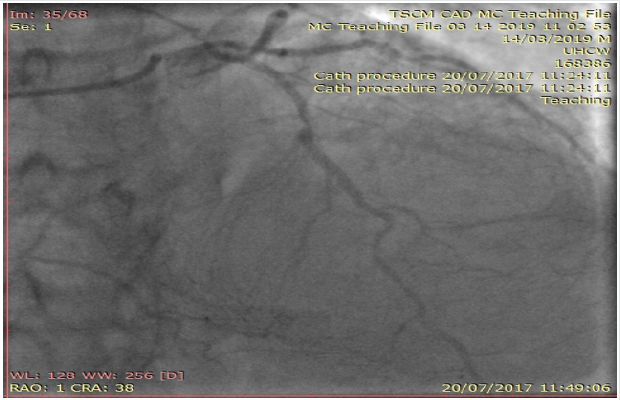
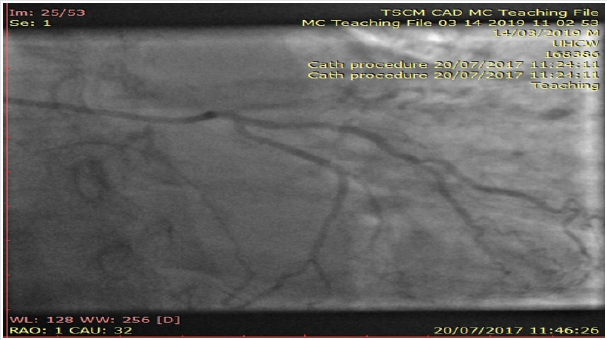
Interestingly, her inpatient coronary angiogram revealed severe
triple vessel coronary artery disease (CAD). This was evident
by the presence of mild disease in the left main stem, severe mid
vessel calcific LAD lesion, severe obtuse marginal (OM1) disease
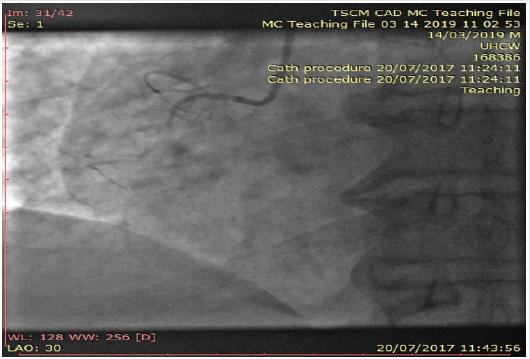
(Figure 3) and chronic total occlusion of her mid right coronary
artery (Figures 4a & 4b). However, her distal RCA appears well
collateralized from contralateral LC system. The left ventriculogram
revealed moderately impaired systolic function with moderate mid
to apical anterior and inferior wall hypokinesis, sparing the basal
segments consistent with “apical ballooning”. Figure 5, LV in systole]
Given her clinical presentation (albeit coronary artery disease
and LV dysfunction), multidisciplinary consensus favored medical
management as NSTEMI. Expectedly patient agreed and preferred
this option too. She was discharged on appropriate treatment and
secondary prevention. Interestingly, her Cardiac MRI (CMR) scan at
1-month post discharge showed near normalization of LV function
with calculated EF 50% with no evidence of infarction or myocardial
oedema or fibrosis. Thence, improvement in her LV function with no
evidence of infarction on CMR confirms the diagnosis of Takotsubo
Cardiomyopathy, despite her significant CAD. At 12-month follow
up, patient still remains stable and symptom free; therefore, with
plans to consider surgical coronary revascularization, if worsening
symptoms on top of medical therapy [2,3].
Figure 3: Coronary angiogram of left system revealing severe mid calcific left anterior descending artery disease with
contralateral collaterals to distal right coronary artery.
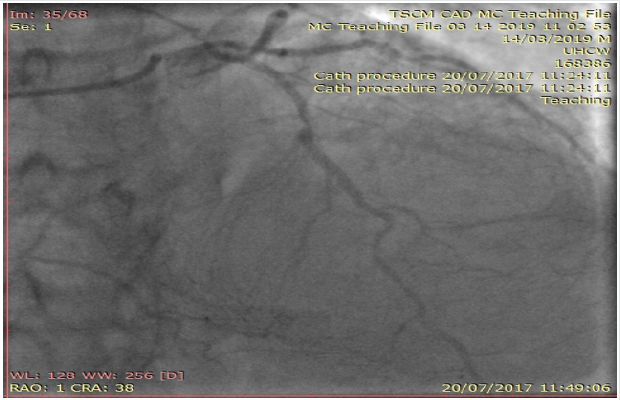
Figure 4a: Coronary angiogram of left system showing severe branch vessel disease in obtuse marginal branch of left circumflex
artery.
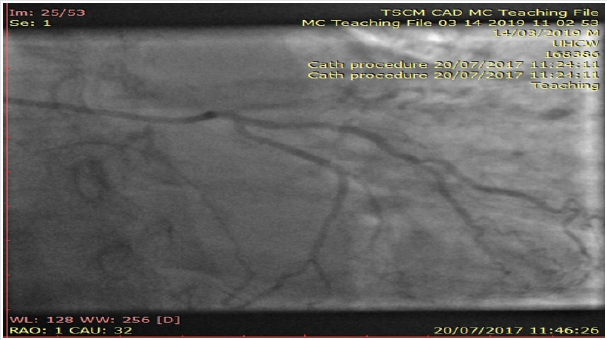
Figure 4b: Angiogram of right coronary artery showing chronic total occlusion at the proximal segment.
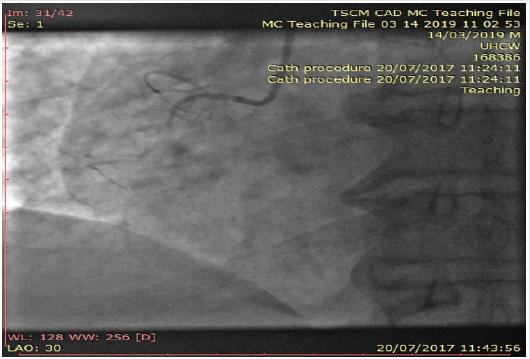
Figure 5: Left ventriculogram at systole confirming the typical pattern of “apical ballooning” sparring the basal anterior and
inferior segments.

Discussion
With her established macrovascular risk factors for CAD
(hypertension and age) and clinical presentation together with
abnormalities in ECG, cardiac enzymes and echocardiogram, the
working differential diagnoses were:
a. Acute Coronary Syndrome (ACS) i.e., Non-ST elevation
myocardial infarction
b. TakotSubo Cardiomyopathy or transient apical ballooning
syndrome or stress induced cardiomyopathy or broken heart
syndrome.
Conventional electrocardiogram (ECG) still remains a costeffective
important tool in the assessment of CAD. Nevertheless,
its low sensitivity (<50%) and specificity (<80%) in predicting
coronary disease still remains a major limitation. Clinicians mostly
rely on surface ECGs to localize ischaemic myocardial territory
(highly specific) prior to coronary revascularization of the culprit
vessel(s) routinely in ACS patients. Clinically TSCM (typical LV
appearance of Japanese “Octopus trap” with apical ballooning)
often mimics AMI (chest pains, elevated cardiac enzymes and
ECG changes) and is characterized by a transient left ventricular
dysfunction. Though its incidence and prevalence doesn’t appear
to have vastly changed over the years; however clinicians are more
comfortable in diagnosing TSCM with better access to imaging
(echocardiogram, Cardiac MRI) and invasive investigations
(coronary angiogram) nowadays. The Revised Mayo Clinic Criteria
suggested the presence of the following to confirm the diagnosis of
TSCM [4,5].
a. Transient hypokinesis, akinesis or dyskinesis of the left
ventricular mid segments with or without apical involvement–
distinctively the extent of regional wall motion abnormalities
observed will be beyond the distribution of single epicardial
coronary vessel and with often a stressful trigger (but not
always present).
b. Absence of obstructive coronary artery disease or
angiographic evidence of plaque rupture
c. New electrocardiographic abnormalities or modest
elevation in cardiac Troponin
d. Absence of pheochromocytoma and myocarditis.
However, concomitant coronary artery disease (CAD) has
been reported in 10 – 29% of patients who have been diagnosed
with TSCM. In the International Takotsubo Registry (n=1750)
15.3% had some degree of coronary artery disease, although
the extent of coronary artery involvement was not discussed in
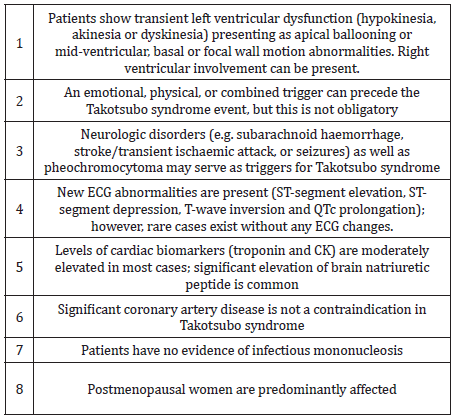
TSCM patients. The new Inter TAK diagnostic criteria highlight
the clinical entity that TSCM can exist with concomitant CAD too
(Table 1). Our patient meets with these diagnostic criteria for
“Takotsubo Cardiomyopathy” together confirming that there was
no evidence of infarction in her Cardiac MRI (no sub-endocardial
late gadolinium enhancement in her LV or microvascular oedema)
as well as complete recovery of her LV function rather than the
initially presumed diagnosis of ACS [6].
The pathophysiology for the condition is not well completely
understood yet; nonetheless, stress related acute catecholaminergic
surge, multi-vessel epicardial coronary spasm, micro-vascular
dysfunction, abnormal fatty acid metabolism, myocardial stunning,
micro-infarction, direct catecholamine toxicity to myocytes
and possible reperfusion injury were proposed as possible
mechanisms. On top of the typical transient apical ballooning, other
atypical variants including inverted or reversed, mid ventricular
or localized have been reported in the literature. In the majority
of cases of suspected TSCM, it is appropriate to perform coronary
angiography to exclude an acute coronary syndrome given the
overlap of symptoms. Also, there is little evidence to support the
clinicians in the management of TSCM with co-existent coronary
artery disease as highlighted in this case and the clinical dilemma
encountered. Therefore, we believe long term follow-up would
be really helpful in understanding the disease as well as their
management and prognosis for these TSCM patients [7,8].
Conclusion
We report an unusual case of Takotsubo Cardiomyopathy
with co-existent severe triple vessel coronary artery disease. This
case illustrates the importance of good history taking and the
judicious use of diagnostic imaging to arrive at a prompt diagnosis
and appropriate management. With limited evidence in literature
to support clinicians as how best to manage these patients with
severe coronary artery disease with Takotsubo Cardiomyopathy,
we highlight the need for International registries with long term
follow-ups.
| https://lupine-publishers-cardiovascular.blogspot.com/ |

No comments:
Post a Comment
Note: only a member of this blog may post a comment.