Lupine Publishers | Journal of Pediatrics and Neonatology
Abstract
Congenital diaphragmatic hernia is a malformation resulting from incomplete fusion of the pleuroperitoneal membrane, it occurs in around 1/5000 live newborns, it produces in the vast majority of cases severe symptoms of respiratory failure and pulmonary arterial hypertension in this age group. Treatment is based on maintaining the best respiratory conditions in the child through intensive neonatal therapy management and, once this objective is achieved, surgical correction of the anatomical defect should proceed. Unfortunately, despite the progress in respiratory management of the seriously ill newborn, mortality from this disease is reported above 75%. We present a case in which the left diaphragmatic hernia associated with pulmonary hypertension led to a fatal outcome in a newborn, despite timely and adequate interventions.
Keywords: Congenital Diaphragmatic Hernia; Pulmonary Hypertension; Respiratory Failure of The Newborn; Surgical Correction
Introduction
Congenital diaphragmatic hernia (CDH) is the most common developmental abnormality of the diaphragm and is one of the most common malformations in the newborn, occurring with a frequency of 1 in 2000 pregnancies and 1 in 2,200 to 5,000 live births. Its presentation is greater in males and is generally located on the left side of the diaphragm, at the site of the Boch dalek foramen, although it is occasionally right (Morgagni foramen) or, with less incidence, it can be bilateral or central [1,2]. The etiology is generally unknown, and most cases are likely to be multifactorial; It has also been associated with chromosomal abnormalities from 20% to 53% and an autosomal recessive form has been described. Despite intense research and aggressive therapeutic intervention in infants with CHD, morbidity and mortality continue to be elevated between 40% and 70% because the hypoplasia and persistent pulmonary hypertension that occur in these patients complicate efforts to maintain a gas exchange with conventional ventilation [3,4].
Case Presentation
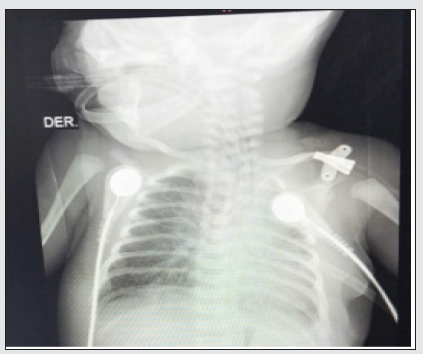
From a nearby municipality, a 37-week-term male newborn was referred to us by Ballard, obtained on 04/16/21 by vaginal delivery without immediate complications. It is the product of the second pregnancy, the son of a 20-year-old mother with a controlled pregnancy twice without ultrasound control. He was born with an APGAR score of 8/10 at 1 minute and at 5 minutes, but at 14 hours of age he presented an episode of apnea with desaturations and generalized cyanosis, requiring positive pressure ventilation and fluid resuscitation with little improvement, due to the persistence of distress. respiratory system, a chest X-ray was performed where intestinal loops were observed in the left lung field, diagnosing diaphragmatic hernia, which is why they were referred to our institution. He was admitted to the neonatal intensive care unit in a fair general condition, cyanotic, hypotonic, desaturated and with a distant audible moan, requiring an orotracheal intubation protocol and invasive mechanical ventilation. The diagnosis was corroborated with a chest X-ray (Figure 1). Orogastric tube was placed to decompress abdominal content, water support and inotropics to maintain adequate mean arterial pressure. He was evaluated by pediatric surgery, who requested presurgical examinations, in which he found prolonged clotting times. Given the instability and the alteration in the coagulogram, surgery was postponed, management with vitamin K was started, and a pediatric hematologist was consulted, who indicated a transfusion of fresh plasma.
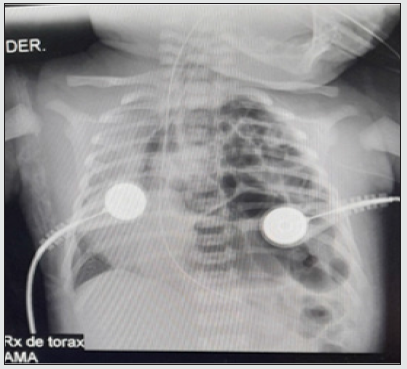
Once his hemodynamic part had stabilized and the clotting times normalized, the patient was taken to surgery on 04/24/21 where a left diaphragmatic defect of more or less 5 cm in diameter was observed and inside the thoracic cavity the presence of small intestine, descending colon, stomach and spleen, for which a reduction of the contents to the abdominal cavity was performed, hernial defect was corrected, diaphragmatic integrity was verified and a chest tube was left, ending the procedure without immediate complications. At 12 hours after surgery, a control X-ray was performed, showing a cardiac silhouette in good position and left lung expansion, and diffuse infiltrates predominantly in the middle lobe were seen in the right lung (Figure 2). An echocardiogram was performed that reported severe pulmonary hypertension with PSAP of 80 mmHg, requiring a phosphodiesterase-5 inhibitor (sildenafil), triple inotropic support and minimal manipulation protocol. Subsequently, a new chest X-ray was performed (Figure 3). Since the newborn presented clinical deterioration, increased work of breathing, generalized mucocutaneous paleness, peri-buccal and distal cyanosis; bradycardia, marked hypotension and desaturation despite established management and high ventilatory parameters. The patient presented cardiorespiratory arrest for which he began advanced cardiopulmonary resuscitation maneuvers for more than 20 minutes without obtaining a response, for which he was declared dead.
Figure 3: Enlarged cardiac silhouette, with enlargement of the atrial cavities and veiling of the left pulmonary trunk, findings suggestive of pulmonary hypertension.
Discussion
The first description of the anatomy and pathophysiology of congenital diaphragmatic hernia was made by Hunter and Mc Cauley in the year 1754; this was defined as the protrusion of the abdominal organs into the thorax, or the descent of the thoracic organs into the abdomen as a result of incomplete closure of the pleuroperitoneal canals. Its incidence is estimated at 1 in 2000 to 5000 births. The defect is more frequent on the left side for 80% and the rest for the right; bilateral ones are extremely rare. The incidence of associated malformations is 10–50% and mortality is high, reaching up to 70% of cases [5,6]. There are reports of high morbidity in patients who survive the initial management of congenital diaphragmatic hernia. Long-term use of mechanical ventilation is associated with bronchopulmonary dysplasia in a higher proportion of children with diaphragmatic hernia. Other types of problems are esophageal ectasia with gastroesophageal reflux in cases of very large defects; recurrence of the hernia or intestinal obstruction are serious complications, although not frequently reported. In a group of patients in which the extracorporeal oxygenation membrane was used, a higher incidence of neurocognitive problems is reported at school [7,8]. Even though there are innovative methods in intrauterine treatment and immediate postnatal therapy, the real solution to this problem will be, in the future, through the knowledge and prevention of the embryological cause and the creation of techniques that induce lung growth [9,10]. In conclusion, this case report brings us closer to knowing this pathology and thus being able to make an early diagnosis and timely management, taking into account its high morbidity and mortality and associated complications.
Read More About Lupine Publishers Journal of Pediatrics and Neonatology Please Click on Below Link:
https://lupinepublishers-pedaitrics.blogspot.com/


No comments:
Post a Comment
Note: only a member of this blog may post a comment.