Lupine Publishers | Journal of Genecology and Women's Healthcare
Abstract
Background: Electrocoagulation during performing laparoscopic ovarian cystectomy as a method used for hemostasis is one of the most commonly and preferred methods due to simplicity and speedy applicability. Fertility outcomes after ovarian cystectomy is a global concern that should be respected and investigated by further research efforts trying to elucidate the best method and protocol in surgical practice.
Aim: To investigate the impact and influence of hemostatic methods implemented in laparoscopic ovarian cystectomy on ovarian reservoir function.
Methodology: A prospective research clinical trial conducted on 72 research study subjects from January 2017 till April 2018. Research study subjects were recruited for the study having unilateral or bilateral ovarian cysts they were equally categorized into research groups according to the hemostatic method implemented during the surgical procedure.
Results: There was no statistical significant difference as regards the ovarian reserve parameters observed before surgery between both electrocoagulation and suture research groups as regards FSH, LH, E2, AMH, AFC, PSV (P value =0.229, 0.063, 0.475, 0.068, 0.609, 0.187 consecutively) after 1 month follow up there was statistically significant difference between suture and electro surgical research groups as regards the FSH, E2, AMH (P values =0.002,<0.001,0.028 consecutively) being more favorable within suture research group ,finally at 6 months follow up there was statistically significant difference between suture and electro coagulation research groups as regards FSH, E2, AMH, AFC, PSV (P values =<0.001, 0.013, 0.023, 0.027, 0.012 consecutively).
Conclusion: Further research efforts are required to evaluate if the difference is clinically significant concerning fertility potential and premature ovarian failure by implementing larger study samples putting in consideration the age and racial differences among the observed cases.
Keywords: Laparoscopic; Ovarian cystectomy; Anti mullerian hormone
Introduction
Ovarian cysts are a frequent form of ovarian lesions that could carry concerns to gynecologists according to their sonographic and histopathological characteristics [1,2].
One of the cornerstone issues and chief factors particularly in child bearing age is the impact of ovarian cystectomy on ovarian reserve function. The hemostatic methods that are implemented during the surgical procedure could influence the functional performance of the ovary at physiological, cellular and molecular levels due to the healing process that follows performance of the hemostatic method [3,4].
Electrocoagulation during performing laparoscopic ovarian cystectomy as a method used for hemostasis is one of the most commonly and preferred methods due to simplicity and speedy applicability. Research debate and many unanswered questions around the clinical and reproductive outcome that various hemostatic methods on ovarian reservoir function such as suturing and electrocoagulation [5,6].
Fertility outcomes after ovarian cystectomy is a global concern that should be respected and investigated by further research efforts trying to elucidate the best method and protocol in surgical practice that would preserve the best ovarian functional reservoir after surgery [7,8].
Aim
To investigate the impact and influence of hemostatic methods implemented in laparoscopic ovarian cystectomy on ovarian reservoir function.
Methodology
A prospective research clinical trial conducted on 72 research study subjects from January 2017 till April 2018. Egyptian research study subjects from Zagazig Governate were recruited for the study having unilateral or bilateral ovarian cysts with good clinical general condition they were equally categorized into research groups according to the hemostatic method implemented during the surgical procedure 36 cases within suture research group and 36 cases within electrocoagulation research group. Inclusive research criteria were as follows in which cases recruited for the research study had an age range 21 to 36 years old, 28-35 days menstrual cycle length; ovarian cyst diagnosis by B- mode sonography; cyst diameter was 5 to 8 cm , no past history of gynecological surgery; no coexisting endocrinological diseases e.g. DM ,hyperthyroidism, and no hormone usage within the previous 6 months before the surgical intervention.
Surgical intervention
After anesthetic induction, the cases have been positioned in supine position, head down and hip up. After classic laparoscopic preliminary steps Pneumoperitoneum have been accomplished observed ovarian cortex covering the cyst wall have been incised in which the ovarian tissue have been observed to be characterized by being thin with few blood vessels. The surgical incision was performed in a manner to be located away from the ovarian hilum anatomical zone. The cyst wall has been stripped off from the normal ovarian tissue using blunt dissection and exteriorized using an endobag. Ovarian tissue hemostasis has been accomplished using bipolar electrocoagulation within the electrocoagulation research group. The probe was in contact with the bleeding points no more than 3 sec, causing the heat to achieve hemostasis. After performing electrocoagulation hemostatic procedure, no suturing was performed for the residual ovarian tissue left, and the ovarian edges have been left to heal by the process of secondary intention. The suture research group ovarian tissue bleeding has been managed by usage of 4-0 absorbable sutures. The surgical incision has been sutured in a manner perpendicular in direction to the ovarian longitudinal axis using a continuous suturing needle was running close to but not via the ovarian cortical tissue.
Ovarian reserve parameters observed
Biochemical 3rd menstrual cycle FSH, LH, E2, AMH were assayed preoperatively,1 month and 6 months after the surgical procedure by using radioimmune assay. Sonographic vaginal color Doppler sonographic assessment after 6 months from performing the surgical intervention the following was obtained as research data to be statistically analyzed involving the following basal antral follicle count in both ovaries (number of antral follicles within early menstrual cycle measuring less than 10 mm in diameter), peak systolic velocity of ovarian stromal blood flow was observed, ovarian volume.
Statistical analysis
Research data was collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. The quantitative data were presented as mean, standard deviations and ranges when parametric and compared between two independent groups using Independent t-test. Also, qualitative variables were presented as number and percentages and compared between groups using Chi-square test and/or Fisher exact test when the expected count in any cell found less than 5. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
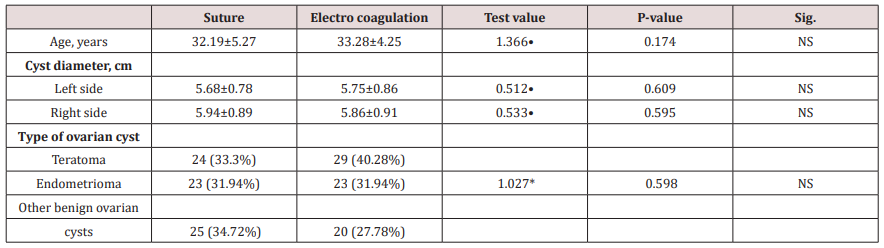
(Table 1) reveals and displays the age, cysts diameters mean +/-SD on left and right sides type of ovarian cysts in which there was no statistically significant differences between both research groups (p values=0.174, 0.609, 0.595, 0.598 consecutively).
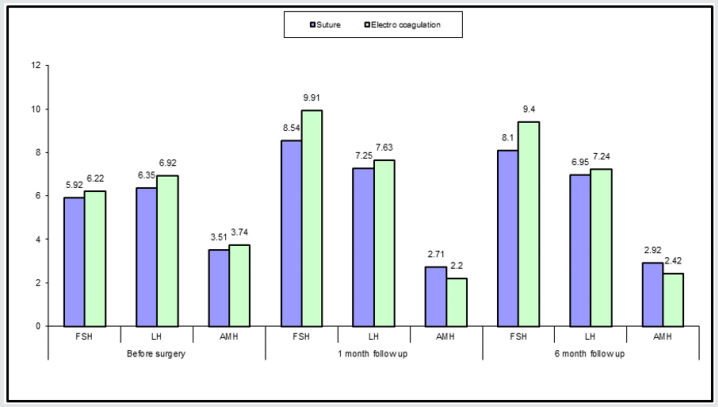
(Table 2) and (Figure 1) reveals and displays the that there was no statistical significant difference as regards the ovarian reserve parameters observed before surgery between both electrocoagulation and suture research groups as regards FSH, LH, E2, AMH, AFC, PSV (P value =0.229, 0.063, 0.475, 0.068, 0.609, 0.187 consecutively) after 1 month follow up there was statistically significant difference between suture and electro surgical research groups as regards the FSH, E2, AMH (P values =0.002,<0.001, 0.028 consecutively) being more favorable within suture research group, finally at 6 months follow up there was statistically significant difference between suture and electro coagulation research groups as regards FSH, E2, AMH, AFC, PSV (P values =<0.001, 0.013, 0.023, 0.027, 0.012 consecutively).
Table 2: Ovarian reserve parameters and indices in suture and electrocoagulation research groups before surgery, 1 month, 6 months after surgery.
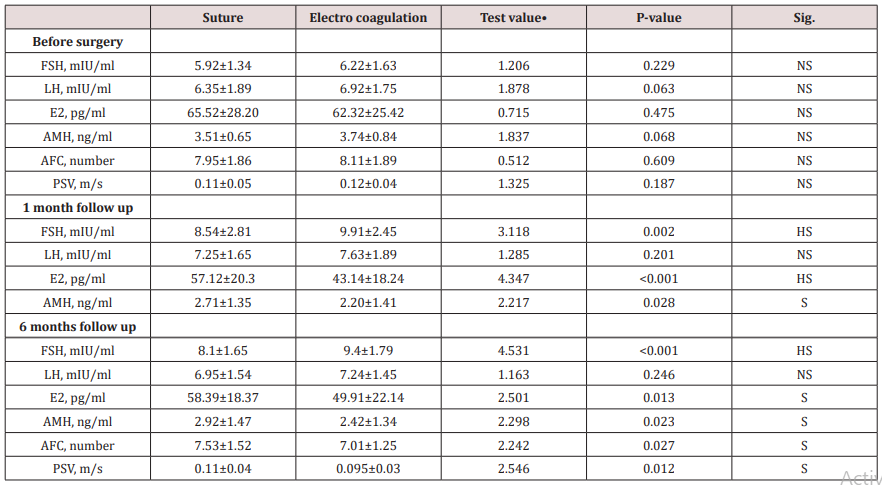
•: Independent t-test
Figure 1: Ovarian reserve parameters in both research groups (FSH, LH, AMH) before ,1 month,6 months after surgery.
(Table 3) reveals and displays that there was no statistically significant difference between both suture and electrocoagulation research groups as regards cyst diameter and pregnancy occurrence within 1 year (p values =0.073,0.729 consecutively).
Table 3: Ovarian cysts diameter and occurrence of pregnancy within 1 year after surgery among both suture and electro coagulation research groups.
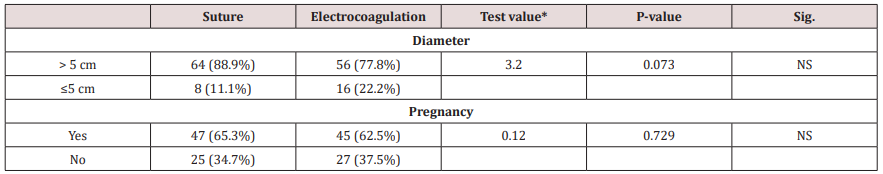
*: Chi-square test
Discussion
Ovarian reserve function after ovarian cystectomy remains the cornerstone research debate issue among infertility practitioners all over the globe, requiring the balance between the best management protocol that preserves the residual ovarian function for infertility management and occurrence of conception after the procedure [9,10].
Hemostatic maneuvers implemented are necessarily required during performance of ovarian cystectomy that needs to have minimal negative impact on ovarian reserve. Ovarian follicular damage and release of inflammatory mediators besides the affection of ovarian vasculature integrity are all proposed negative impacts that could affect the ovarian function particularly after ovarian cystectomy [11,12].
Reproductive potential of cases is measured by various indices and parameters that reflect the ovarian function such as Anti mullerian hormone, antral follicular count, peak systolic velocity among others are affected by age and surgical interventions affecting the ovarian structural integrity [13,14].
There is no single assay that could reflect ovarian reservoir function with 100% precision. Integrated assessment of various parameters and indices have shown by various prior research groups of investigators to be more precise for ovarian reserve predictability [15,16].
Interestingly a prior research systematic review compared and contrasted the impact of suturing and surgical energy hemostasis implemented during ovarian cystectomies on ovarian reserve function statistical analysis of the pooled research data powerfully supports the usage of suturing rather than surgical energy (e.g. bipolar coagulation) for hemostasis since it offers enhanced ovarian function preservation during ovarian cystectomy. In which ovarian reserve markers AMH, AFC, PSV, ovarian volume have been revealed and displayed to have a positive correlation to suturing usage the research team of investigators in harmony and similarity to the current research study findings have revealed that suturing for ovarian cystectomy hemostasis is superior to electrocoagulation for ovarian function preservation [1,3,7].
A previous similar research study to the current study investigated, suturing and electrocoagulation as hemostatic methods, to control ovarian wound bleeding during laparoscopic ovarian cystectomy performance, and assessment of ovarian reserve after intervention was conducted by the research team of investigators. The serum levels of E2, FSH and AMH have statistically significant at 1- and 6-months post procedure between both research groups (P values <0.05). Further more it was observed that the blood flow of the ovarian stroma, antral follicular count and peak systolic velocity post- procedural indices among the electrocoagulation research group was lower in comparison and contrast to the suture research group, in a statistically significant fashion (P values <0.05). The research team to the conclusion that hemostatic suturing during laparoscopic ovarian cystectomy is superior in maintenance of the follicles and cortical blood supply within the residual ovarian tissue. on the other hand, electrocoagulation hemostasis caused a reduction in of ovarian functional performance in a more considerable manner than hemostatic suturing. those research findings in addition show great harmony and similarity to the current research study findings [4,6,15].
Conclusion and Future Research Recommendations
Further research efforts are required to evaluate if the difference is clinically significant concerning fertility potential and premature ovarian failure by implementing larger study samples putting in consideration the age and racial differences among the observed cases.
Read More About Lupine Publishers Journal of Gynaecology Please Click on Below Link:
https://lupinepublishers-gynecology.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.