Lupine Publishers| Online Journal of Neurology and Brain Disorders
Abstract
We report the first-ever case of left fronto temporal-onset seizures causing ictal a systole, within 24 hours of a left sphenoid wing meningioma resection. It reinforces the importance of close monitoring of neurosurgical patients with continuous EEG.
Keywords: Seizure; A systole; Meningioma; Case report
Introduction
Autonomic dysfunction in various forms, affecting the cardiovascular, respiratory, gastrointestinal and other systems, is commonly associated with seizures. Seizures frequently affect the heart rate and rhythm, often in a transient manner. An increase in heart rate is very common with various kinds of seizures, but ictal bradycardia and a systole are much less common [1]. Symptomatic ictal Brady arrhythmias occur in less than 0.5% of epilepsy patients, and the overwhelming majority have been reported in association with temporal lobe epilepsy. The common presentation is a patient who has complex partial seizures with or without secondary generalizations, who develops ictal a systole and syncope. It has been suggested that this is a seizure self-termination mechanism [2].
We report here a case of a woman with new onset seizures caused by a meningioma, who had episodes of ictal a systole following tumor resection. To our knowledge, this is the first-ever report of ictal a systole that began after tumor resection - most cases in the literature noted this in the setting of long-standing temporal lobe epilepsy. While illustrating the importance of the central autonomic network in cardiac function, it also emphasizes the need for neurosurgical patients to be closely monitored following their procedure.
Case Report
A 69-year old female with diabetes mellitus with a newly- diagnosed left sphenoid wing meningioma was admitted to our hospital for resection. The meningioma had been diagnosed after she had developed new-onset seizures a month prior to admission. She had been started on levetiracetam for seizure prophylaxis. Her admission labs were significant for elevated glucose, and mild hyponatremia of 128mill moles per liter, that corrected to 135mmol/L when adjusted for elevated glucose level.
After an uneventful left craniotomy and mass removal, she remained in the intensive care unit for monitoring. Late in the evening on the day of her surgery, she had an episode of bradycardia progressing to loss of pulse, for which cardiopulmonary resuscitation with chest compressions was initiated. However, she regained spontaneous circulation quickly. She was showing some confusion and altered speech, and therefore had a long-term EEG placed to rule out seizure. The EEG was significantly asymmetric, with attenuation, slowing, and rare trains of epileptiform activity over the left hemisphere. She had another episode of loss of pulse, requiring cardiopulmonary resuscitation through chest compressions, with the spontaneous return of circulation within 1 minute. EEG revealed subtle left frontal seizure preceding the asystole that quickly spread to the contra lateral hemisphere. Subtle left arm and head jerking were the only other clinical correlate. Diffuse EEG suppression followed the a systole.
She was started on a dopamine infusion, but the next morning she had two more episodes of asystole lasting 15 and 10 seconds in rapid succession. There was EEG evidence of left fronto temporal onset seizures with rapid progression to involve the contra lateral side preceding this asystolic event. There was also evidence for fontal rhythmic intermittent delta activity (FIRDA) on the left, a nonspecific finding that might indicate increased intracranial pressure or other frontal dysfunction. A temporary transvenous pacemaker was implanted. She had an episode of supra ventricular tachycardia, but remained otherwise stable.
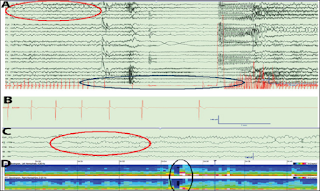
Figure 1: (A) Standard scalp EEG sampled at 500 Hz, time compressed at 2mm/sec and viewed with filter 1-70 Hz. The red circle denotes onset of a partial seizure in the left temporal region. The blue circle highlights asystole lasting 56 seconds. (B) Single lead EKG demonstrating bradyarrythmia leading to asystole. (C) left temporal chain electrodes demoinstarting seizure onset. (D) Time compressed FFT (1-40Hz) - left hemisphere over right hemisphere. The black circle highlights the abrupt flattening of EEG following asystole.
Increasing the daily levetiracetam dose and correction of hyponatremia with hypertonic saline led to the cessation of epileptiform discharges on the EEG. However, her affect remained flat, and the decision was made to taper the levetiracetam and start oxcarbazepine. Her seizures remained under control, and no further brad arrhythmias were noted, leading to the removal of the temporary pacemaker five days after it was inserted. The patient was discharged to a rehabilitation facility and remained stable at follow-up (Figure 1).
Discussion
The cause of ictal Brady arrhythmias is debated. There does not seem to be any evidence for primary cardiac conduction defects. It has been suggested that the fact that there are delays between seizure onset and a systole that the pathology involves activation of certain brain regions [2]. It is known that there is a central autonomic network in the brain, of which the insula is a part, and stimulation of areas within it can trigger parasympathetic outflow changes. Catenoix et al. [3] stimulated the insula in human subjects, causing high-frequency discharges there, which were followed by a systole after 2 seconds. A direct postganglionic effect on the heart is possible, which may tend to synchronize autonomic input to the heart with epileptic activity [4].
The insula is a deep structure, and scalp correlate to an insular seizure is likely to be a frontal or a temporal ictal discharge. In our case, subtle but unequivocal left frontotemporal rhythmicity preceded the a systole in both events. It was otherwise absent from the record. It is feasible to postulate that left frontal seizures originating from a known lesion reached the insula, and caused cardiac pause and/or a systolic arrest.
There are some studies which suggest that autonomic control, especially as mediated by the insula, shows hemispheric lateralization, with the right hemisphere predominantly modulating sympathetic tone, and the left hemisphere parasympathetic tone [5]. However, studies on ictal arrhythmias have not been consistent in their findings concerning lateralization [2]. Therefore, the question of what makes certain epilepsy patients prone to Brady arrhythmias and a systole, as opposed to tachy arrhythmias, remains open.
Conclusion
This first report of ictal a systole following meningioma resection reinforces the need for close monitoring of neurosurgical patients, especially with EEG, and being alert to the possibility of a systole and syncope in those with fronto temporal seizures. The brain-heart connection as represented by the central autonomic network's influence on cardiac function needs to be further investigated.
Read more about Online Journal of Neurology and Brain Disorders please click on below link https://brain-disorders-lupine-publishers.blogspot.com/
No comments:
Post a Comment
Note: only a member of this blog may post a comment.