Lupine Publishers | Journal of Clinical & Community Medicine
Abstract
Aim: The purpose of this study was to identify whether appropriate consent was obtained for taking collateral histories and whether there was evidence of differences between two ethnic groups.
Method: Case records of in-patients were reviewed. A sampling framework was established for the identification of 20 in-patients aged over 65 years. Five English and Asian men, as well as 5 English and Asian women were selected from 4 medical wards.
Results: The average age of men and women and of English and South Asian patients was comparable at about 80 years. The lowest standards were achieved in scoring cognition and identification of the source of any collateral history. For South Asian patients the preferred language of the patient was only noted on three occasions When score rates were compared the average standard score for English patients was 4.1out of 6 compared to 2.8 for South Asians.
Conclusion: We need to provide staff with detailed guidance at induction and during junior training sessions as to when and how collateral histories should be taken and the legal requirement to document such details.
Introduction
The need to obtain a collateral history places an additional burden on busy clinical staff and is even the subject of Twitter discussions. Sommer [1] Questions as to patient confidentiality can raise additional difficulties. When the patient does not feel at home in English it is easier to accept a simple Yes or No to a series of questions and to believe the responses are correct, than to seek out a translator who will appreciate the subtleties of patient confidentiality. Such communication problems make any formal assessment of cognition difficult and why should someone who grew up outside of Europe know the exact dates of World War II when the partition of India and Pakistan is of considerably more personal relevance?
Against this background we should question whether collateral histories are of value. Research has shown that they can:
a) Help minimise risk factors.
b) Mobilise family and friends to help with aftercare.
c) Overcome problems caused through confabulation,
misunderstanding and language issues.
Nevertheless, the patient’s consent to obtaining such information should be sought and documented in the notes. Beedle [2] Such discussions with caregivers are also likely to identify stress to which they are subject and may have a direct impact on the clinician’s ability to discharge a patient.
Method
Standards for collateral histories were developed after
discussions with consultants working in general medicine and
medical care of the elderly. These standards were
a) That a formal check on cognition should be recorded. This was
considered essential for patients aged over 75 years.
b) That a collateral history was obtained within 2 days of
admission.
c) The source of the collateral history was recorded
d) The preferred language of the patient was recorded
e) The collateral history included details of any package of care,
the nature of accommodation, issues concerned with washing
and dressing, Day Care and Meals on Wheels.
f) Information on mobility was recorded
Each of these 6 standards was considered mandatory.
In addition, details were collected on who took the collateral history and where the preferred language was not English was a translator used and if so, who was that translator.
A sampling framework was established for the identification of 20 in-patients aged over 65 years. The selection of cases was for 5 English and 5 Asian men, as well as 5 English and 5 Asian women. Medical wards were visited in turn and pro-forma completed. As soon as a quota was reached no further notes were reviewed in that category. The day of review was midweek and 4 medical wards were visited in succession. In each ward appropriate patients were identified in sequence and pro-formas completed.
Subsequent to the audit an educational program was delivered to doctors working on these medical wards with the intention of improving the methods of obtaining collateral information and its quality. The educational program consisted of unit meetings and lectures. Six weeks after the initial assessment and educational program a repeat audit was initiated on the same medical wards using the same methods of data collection.
Results
Eight men were identified on Ward A, 4 women on Ward B, 0 patients on Ward C, 2 men and 6 women on Ward D. The average age of men and women and of English and South Asian patients was comparable at about 80 years. Eight of the English patients and 8 of the South Asian patients were over 75 years old.
The lowest standards were achieved in scoring cognition and the identification of the source of any collateral history. (Tables 1 & 2) Both of these failures call into question the validity of both patients provided histories and any collateral history that was obtained. This is especially true for South Asian patients where the preferred language of the patient was only noted on three occasions and a translator only made available in two cases. (Table 1) The inadequacy of such assessments in most cases was emphasized by comments made by nurses who often stated that patients for whom these details were not recorded had a limited knowledge of English or none at all.
Table 1: A Spot Audit of Collateral Histories taken on the Medical Wards at Leicester Royal Infirmary.
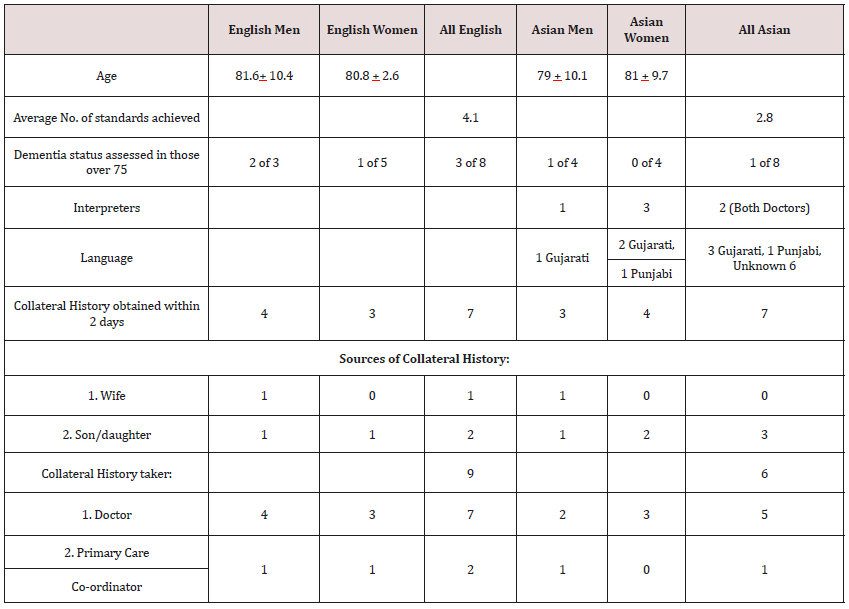
Table 2: Recording of individual standards achieved during audit of collateral history: * It was assumed that for all English patients English would have been the preferred language.
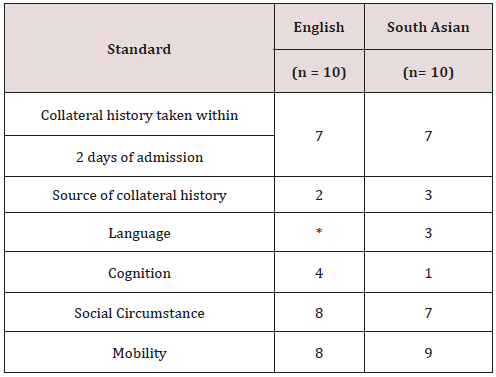
When score rates were compared between English and South
Asian patients using Stats Direct software there were no statistical
differences as the population size was small. However, the average
standard score for English patients was 4.1out of 6 compared
to 2.8 for South Asian patients. This difference almost reached
significance with t = 1.49, p < 0.08.
Other qualitative data which emerged from the audit included:
a) The only professional translation provided for patients with
limited English skills was by two doctors.
b) None of the three entries for collateral histories taken by a
Primary Care Co-ordinator were signed or dated.
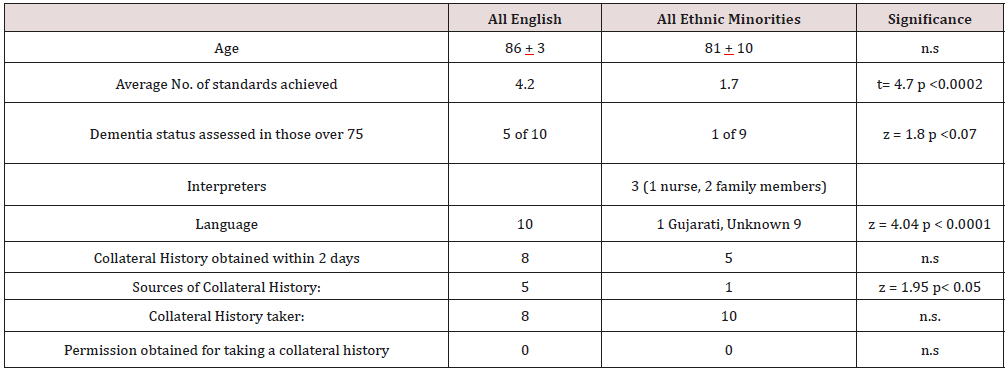
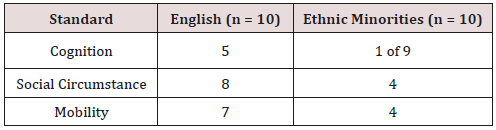
At the re-audit there was little evidence of any beneficial effect
from the interventions. In particular, patients from ethnic minorities
continued to have significantly fewer assessments of dementia
status. (Table 3) There was also a failure to use professional
translators or identify the source of collateral histories amongst
patients from ethnic minorities recorded in the clinical record.
Table 3: A Spot Re-audit of Collateral Histories taken on Medical Wards at Leicester Royal Infirmary.
Discussion
The standard of collateral histories needs to be improved. The main changes that should be incorporated into future clinical histories should include:
a) Documentation of a discussion with the patient of the need for
a collateral history.
b) The provision of a translator who has an understanding of the
issues of confidentiality when the patient’s preferred language
is other than English.
c) Formal checking of cognition and recording scores for all
patients over 75 years.
d) Ensuring that all entries are signed and dated.
e) Statements to explain why standards have not been completed
when this arises.
In order to achieve these outcomes, we need to provide staff with detailed formal guidance at induction and during junior training sessions. Simple educational programs and talks at unit meetings are not effective. There is a need to introduce mandatory e-based training programs with formal assessments. There may also be a place to encourage junior doctors to use formal pictograms which would cover items such as the nature of housing, mobility and the provision of food together with the role of careers. Pictograms have been popularized through use on the worldwide web and in software. Better known as “icons” they are displayed on a computer screen in order to help the user navigate a computer system or mobile device. Otto Neurath, Austrian philosopher of science, was one of the influential minds behind graphic representation of data. A strong believer in visual education, he held the view that by using simplified symbols (pictograms or icons), viewers could, at a glance, understand complex information regardless of their education.
Their introduction into the clinical record could have significant benefits for conveying vital information about housing, mobility and dependence. The introduction of a limited number of specific pictograms covering these aspects of social history could ensure uniformity through a shared understanding by clinicians of what each sign means.
The second issue which emerged clearly from these studies was the inadequacy with which elderly patients from ethnic minorities were assessed. Leicestershire has a large South Asian population, mainly of Gujarati and Punjabi origin. Most families came to the area in the 1970s. However, amongst the older population there are a substantial number of people whose language of choice is still Gujarati, Punjabi or Urdu. Despite a long-standing commitment to improved patient communication in these communities [3,4] the current situation is inadequate. The belief of the Care Quality Commission during its in-depth inspection of University Hospitals of Leicester NHS Trust in 2014 [5] that cultural diversity and social deprivation of the community is well served appears to be illfounded. Its report states:
“We spoke with staff about how they communicated with people whose first language was not English. They told us they had access to a telephone interpreter service (Language Line) and that many staff were bilingual or multilingual and could be used to interpret. We did not see evidence that communication was an issue at this trust.”
The need to ensure adequate access to linguistic support is well recognized, especially amongst elderly patients [6]. However, in practice this clearly remains a problem and needs to be urgently addressed. A lack of accurate knowledge obtained through informed collateral histories is clearly a significant cause of delayed discharges across many communities [7].
Acknowledgement
This study was a registered audit (7521) of University Hospitals of Leicester NHS Trust.
Read More Lupine Publishers Journal of Clinical & Community Medicine Please Click on Below Link:
https://journalofclinicalcommunitymedicine.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.