Lupine Publishers | Journal of Reproductive System and Sexual Disorders
Abstract
Klinefelter syndrome patients are mostly clinically azoospermic, and before the era of TESE, were unable to father genetically their own offspring. Nonmosaic Klinefelter [NMK] patients have chances of fatherhood once sperm is harvested from the epididymal seminiferous tubules and further injected in the ovarian cytoplasm. We report a case of 36y old NMK patient, treated for 3 months with supportive and hormonal medication achieving a pregnancy after TESE/ICSI. This is the first published case of successful conception in a couple with a nonmosaic Klinefelter father in Egypt using TESE/ICSI. Review of the literature for any advantages of mTESE over TESE and conception demonstrated higher pregnancy rates by TESE although the sperm retrieval rate was similar in both techniques.
Conclusion: Nonmosaic Klinefelter patients should no longer be considered sterile.
Keywords: Klinefelter Syndrome; Azoospermia; Male Infertility; TESE; ICSI
Introduction
Klinefelter syndrome [KS] was first described in 1942 by Harry Klinefelter [1]. It is the most common chromosomal disorder in men. The estimated prevalence of K Sis 0.2% in the general population, 3% among infertile men, and up to 11% in men with non-obstructive azoospermia [2]. Yet, KS remains frequently under diagnosed, because of the wide phenotypic variation among affected individuals, and the lack of established screening programs. Only 25% of men with KS are diagnosed during their lifetime, with fewer than 10% being diagnosed before puberty [3]. The disorder is categorized by X-chromosome polysomy, with X-disomy [47, XXY] being the most common variant representing about 85%- 95% of the cases. Characteristic features of KS include small testes, hypogonadism, and infertility [4]. Higher grades of X chromosome polysomy are associated with a more severe clinical presentation, whereas genetic mosaicism (46, XY/47, XXY) usually results in a milder phenotype [5].
Since the introduction of intra-cytoplasmic sperm injection [ICSI] [6] and testicular sperm extraction [TESE] [7], a considerable number of men with Klinefelter syndrome have been able to father genetically own offspring. Looking at the three of the more recent published studies, in 2015 Ozveri et al. [8] confirms that sperm retrieval is possible in azoospermatic Klinefelter Syndrome patients, and recommends the use of artificial reproductive techniques (ART) for those wishing to conceive. In 2016 Ishikawa et al. [9] concluded that the use of mTESE to extract motile sperm is vital in the use of Klinefelter Syndrome cases in order to maximize the chances of achieving a clinical pregnancy and embryological development. In 2016 Vicdan et al. [10] concluded that with regards to the use of fresh vs. cryopreserved sperm in ICSI cycles demonstrated an equal chance of success. In this case report a successful conception in an azoospermic nonmosaic Klinefelter father using a combined TESEICSI protocol is highlighted.
Case Presentation
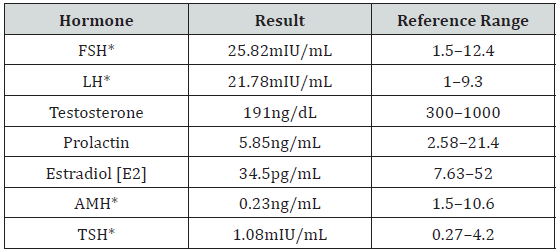
A 36 year old Egyptian male of rural origin presented to our fertility clinic complaining of primary infertility for 9 years. He enjoyed a good sex life, without any concern regarding libido, erection, intercourse and ejaculation. His wife was 10 years younger and her menstrual history was unremarkable. General examination diagnoses well developed secondary male sexual characteristics, 187cm tall and weight of 82Kg. Genital examination revealed an average sized penis with normal male pubic hair pattern and two small firm testicles. Both vas were palpable and showed no abnormality. Repeated spermo grams in 3 months intervals and 3 days of abstinence diagnose total azoospermia. The second result was a duplicate of the first one and the results of the hormonal assay showed a hypergonadotrophic hypogonadism state (Table 1). Karyotyping followed clinical data, raised suspicion of Klinefelter Syndrome, reporting a nonmosaic Klinefelter (Figure 1).
*FSH=Follicle Stimulating Hormone, LH=Luteinizing Hormone, AMH=Anti-Mullerian Hormone, TSH=Thyroid Stimulating Hormone.
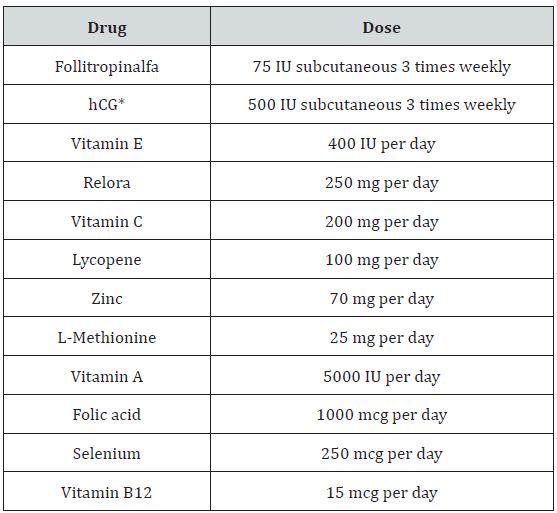
Although the value of treatment of cases with hypergonadotrophic hypogonadism is controversial, the patient was treated for 3 months with combined hormonal and nonhormonal supplement therapy prior to TESE (Table 2). An attempt to enhance the harvest of the scheduled testicular sperm extraction and improving ICSI chances of fertilization. TESE was performed and multiple sections were retrieved from both testes. Primary scanning of the surgical harvest revealed azoospermia. After processing, the left testis showed motile sperms from 2 tissue cores, allowing for ICSI as well as a cryopreservation vial for future interest. The operation was uneventful. Postoperatively mild left orchitis was diagnosed which subsided after a 10day course of quinolones, anti-inflammatory drugs and scrotal elevation.
The wife was treated with long GnRH agonist regimen, pituitary down-regulation with Triptorelin 0.1mg once daily SC injection [decapeptyl;Ferring], commenced in the midluteal phase of the menstrual cycle and continued for 2 weeks. This was followed by estradiol blood level and Trans vaginal ultrasound confirmation of down-regulation, recording the leading follicle diameter and antral follicular count [AFC]. Human menotropin, gonadotropin injections at a dose of 225IU/day [menogon;Ferring] initiated and continued until leading follicle reach 24mm maximum diameter, within high range estradiol level and low progesterone level. The hCG injection [Choriomon 5000 IU/day; IBSA; Egypt] was administered when at least three follicles reach R17 mm in diameter. Vaginal egg collection was scheduled 36 hours following hCG triggering. TESE was performed before oocyte retrieval in order to confirm a positive retrieval of sperms. Microscopy of the retrieved semen isolated 28 out of total 58 spermatocytes. The rest were either immotile or with sluggish tail movement. Overall 22 oocytes were retrieved while 15 diagnosed at MII stage. ICSI was performed and 6 good quality A and B embryos progressed to day 3. Three embryos at stage A were transferred on day D3. Twelve days post ET the beta hCG was 141.0mIU\m. The lady delivered at term, a healthy female baby of 3000gr.
Discussion
Historically, men with KS were considered infertile. However, it is now well accepted that isolated foci of spermatogenesis can exist in the testes of patients with KS [11]. This discovery, along with advances in assisted reproductive technologies [ART] during the past two decades, has made paternity possible for men with KS. Surgical sperm retrieval and intracytoplasmic sperm injection [ICSI] have dramatically improved the fertility potential of men with KS. Tournaye et al. first reported on successful sperm retrieval in men with KS using TESE in 1996 [12]. The first pregnancies achieved using ICSI of ejaculated and testicular sperm were reported 2 years later [13]. Since then, there have been reported 101 children born to fathers with nonmosaic KS [14].
With the use of micro dissection TESE, sperm retrieval rates in patients with KS are considered equivalent to those in men with non-obstructive azoospermia. The outcome of mTESE versus TESE in non-obstructive azoospermia was also investigated by a systematic review published in 2014. Seven out of 62 identified studies were included in the final analysis. SRR was significantly higher in the mTESE group (42.9-63%) in comparison with TESE (16.7-45%) [15]. In another retrospective cohort study among 714 men with NOA, 40.5% had successful sperm retrieval at their first TESE. In total, 261 couples had 444 ICSI cycles and 48 frozen embryo transfer cycles, leading to 129 pregnancies and 96 live birth deliveries. The expected cumulative delivery rates after six ICSI cycles were 78%.Authors indicated the intrinsic limitations related to the retrospective cohort study design [16]. Our recent published, review results demonstrate among 1,070 KS patients treated by ICSI the SRR was 46.3% and PR was 21% with mTESE and 45.6% SRR and 44.4% PR with TESE [17]. Fewer complications were observed on ultrasound examination after mTESE procedure [15].
Mehta A et al. [18] published a systematic review/metaanalysis to investigate the effect of early hormonal therapy [HR] on sperm retrieval rates in patients with Klinefelter Syndrome [KS]. Although the studies varied in their conclusions as to predictors of sperm retrieval, positive predictors included young age and preoperative Testosterone levels close to or within the normal range, either at baseline or with hormonal therapy [aromatase inhibitors, clomiphene citrate [CC], or hCG] [19-22] Several authors have identified ‘‘young’’ patient age, usually defined as age <30 years, as being the most consistent positive predictor of sperm retrieval in patients with KS [23,24]. The age of the reported patient was 36 years who does not fit with most the studies age predictor for successful retrieval. However, his testosterone level was low and the treatment before surgery might have had a positive impact upon successful sperm retrieval.
Conclusion
The majority of 47, XXY males are azoospermic and considered sterile until the introduction of TESE/ICSI. Solid parameters to distinguish patients with KS and fertilization potential and chance of fatherhood are missing. A prospective randomized control study would probably reveal those important parameters indicating KS patients with higher chance to achieve a pregnancy.
Read More About Lupine Publishers Journal of Reproductive System and Sexual Disorders Please Click on Below Link:
https://lupine-publishers-reproductive.blogspot.com/


No comments:
Post a Comment
Note: only a member of this blog may post a comment.