Lupine Publishers| Journal of Neurology and Brain Disorders
Abstract
Postoperative oculomotor nerve palsy is a rare complication that occurs in the setting of micro¬surgical aneurysm clipping. While a number of theories have been postulated to explain the development of postoperative oculomotor nerve palsies, the underlying pathophysiology of such complications still remain to be elucidated. In this report, we present a case of postoperative isolated ipsilateral oculomotor nerve palsy after clipping of basilar tip aneurysm which we believe may be attributed to periperative oculomotor nerve manipulation related neuropraxia.
Keywords:Oculomotor Nerve Palsy; Basilar Apex Aneurysm; Postoperative
Introduction
Oculomotor nerve is the third cranial nerve that enters the orbit through the superior orbital fissure and controls muscles that drive most movements of the eye and raise the eyelid. Oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in the control of eye movement. Oculomotor nerve palsy is an eye condition resulting from damage to the third cranial nerve or a branch there of. As the name suggests, oculomotor nerve supplies the major¬ity of the muscles that control eye movements. Therefore, damages to oculomotor nerve will render affected individuals unable to move his or her eye normally. Unilateral oculomotor nerve palsy is often encountered in the setting of ipsilateral aneurysms located at the Posteri¬or Communicating Artery (PcomA), Internal Carotid Artery (ICA) or their junction (PcomA/ICA). There have been some reports on ocu¬lomotor nerve palsy as a result of aneurysms in basilar tip, anterior artery or anterior communi¬cating artery. In the present report, we describe a case of basilar apex aneurysm presenting with ipsilateral postoperative oculo¬motor nerve palsy that is thought to be attrib¬uted to peroperative oculomotor nerve handling followed by neuropraxia.
Case Report
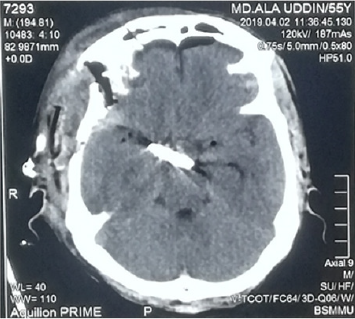
A 55years old hypertension male with no other significant past medical history or contributing family history complained about sudden severe headache for one hour followed by several episodes of vomiting and unconsciousness for 05 hours on admission at our hospital. Physical examination results were within nor¬mal limits except for considerable neck stiffness, positive Kernig sign and Brudzinski’s sign. Computed Tomography (CT) scan demonstrated diffuse subarachnoid hemorrhage, which was especially concentrated in ambient, sylvian fissure, interpeduncular and suprasellar cisterns with intraventricular extensions and mild triventricular hydrocephalus (Figure1). Computed tomography of the head show¬ing diffuse subarachnoid hemorrhage especially concentrated in ambient, sylvian fissure, interpeduncular and suprasellar cisterns with intraventricular extensions and mild triventricular hydrocephalus. CT Angiography (CTA) revealed a large saccular basilar tip aneurysm (approximately 10.7×9.5×10.5mm) (Figures 2A & 2B). The aneurysm was micro surgically clipped (Figures 4) via the right Orbitozygomatic approach (Figures 3A & 3B). Postoperatively the patient developed complete right third nerve palsy characterized by the presence of dilated pupil, ptosis and downward deviation and abduction of the eyeball. CT scan revealed no postoperative intracranial hematoma and the surgical clip was in the proper location. However, compression of the basal cisterns and assessment of the ventricular system were noted (Figure 5). Postoperative CTA showed no existence of another aneurysm or vasospasm (Figure 6). The patient was discharged 02 weeks after the surgery. At this point, his mydriasis and eye lid drooping were still present to a lesser extent. At one-month follow-up, the patient’s pupil was slightly contracted and reflexed reluctantly to direct and indirect light stimulation.
Figure 1: Computed tomography of the head show¬ing diffuse subarachnoid hemorrhage especially concentrated in ambient, sylvian fissure, interpeduncular and suprasellar cisterns with intraventricular extensions and mild triventricular hydrocephalus.
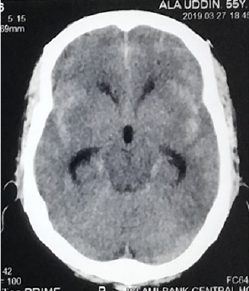
Figure 2A & 2B: Computed tomography angiography show¬ing a large saccular basilar tip aneurysm (approximately 10.7×9.5×10.5mm). The arrow indicates the aneurysm.
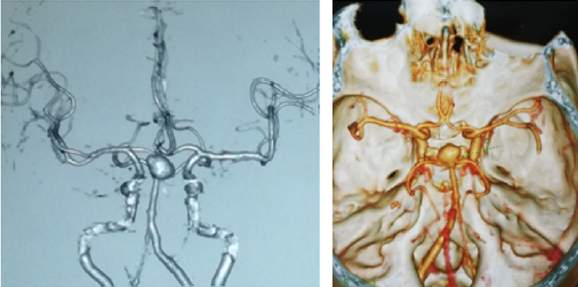
Figure 3A & 3B: Right sided Orbitozygomatic craniotomy (one piece), extradural anterior clinoidectomy & clipping of basilar apex aneurysm through trans-sylvian approach.
Figure 6: Postoperative CTA showed no existence of another aneurysm or vasospasm and the surgical clip was in the proper location.
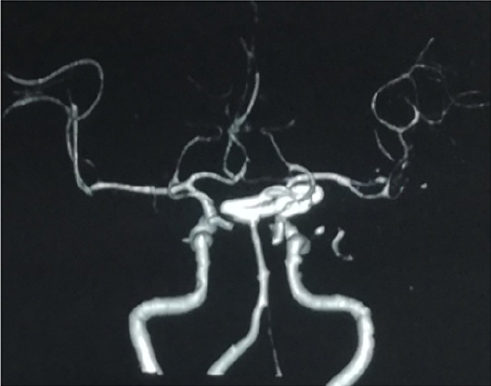
Figure 7: On postoperative day two, the patient developed a complete right third nerve palsy.
Discussion
There are many proposed hypotheses pertain¬ing to the etiology of oculomotor nerve palsy before and after aneurysm surgery. Direct com¬pression by the aneurysm is the most classic and common cause. Other causes include direct injury to the third nerve intraoperatively [1-6], microvascular ischemia [7-9], focal hemato¬ma formation [3], vasospasm [8-12], anomaly of the vessels along the oculomotor nerve [10], elevated intracranial pressure and herniation, compression by intracranial structures other than aneurysms [7], and undetermined ori-gins [11]. In the present case, compression by aneurysm may not be possible because of the anatomi¬cal distance between the two entities. Postoperative CT, CTA decrease the chances of hematoma formation, vasospasm and elevated intracranial pressure. Although we cannot rule out the possibility of ischemic injury to the oculomotor nerve. Small vessel ischemic injury to oculomotor nerve usu¬ally exhibits pupilsparing [9] whereas our patient demonstrated a blown pupil. So, we believe that, probably from coarse dissection of the cavernous sinus dura and as well as direct anterior clinoidectomy or from heat of the low power drill may be responsible for the 3rd nerve palsy of our patient.
Conclusion
The novel use of intramuscular cerebrolysin and citicoline in a patient with kernicterus was safe and effective.
The Neuroreparative Effects of Cerebrolysin have Been Attributed to [3-5]:
a) Inhibition of apoptosis.
b) Improving synaptic plasticity and induction of neurogenesis.
c) Augmenting the proliferation, differentiation, and migration of adult.
d) subventricular zone neural progenitor stem cells, contributing to neurogenesis.
e) Induction of stem-cell proliferation in the brain.
Citicoline (cytidine diphosphate choline) is a mononucleotide made of ribose, pyrophosphate, cytosine and choline is a watersoluble naturally occurring substance that is generally grouped with the B vitamins. It is also considered a form of the essential nutrient choline. It is a safe substance with generally minor side effects which may include digestive intolerance after oral administration [6]. An accumulating research evidence suggests that citicoline is endowed with interesting pharmacological properties that can make it useful in the treatment of various disorders that has no universally accepted effective treatment including neurological conditions such as Parkinson’s disease, brain ischemia, hemorrhagic stroke, Alzheimer’s disease; and ocular condition such as glaucoma, nonarteritic ischemic neuropathy and amblyopia [6].
The Neuro-Protective Effects of Citicoline Were Attributed to the Followings [6]:
a) Preservation of cardiolipin and sphingomyelin
b) Preservation of arachidonic acid content of phosphatidylcholine and
c) phosphatidylethanolamine.
d) Partial restoration of phosphatidylcholine levels.
e) Stimulation of glutathione synthesis and glutathione reductase activity.
f) Reduction of phospholipase A2 activity.
g) Increasing glucose metabolism in the brain.
h) Increasing cerebral blood flow.
Reducing oxidative stress and preventing excessive inflammatory response in the brain by inhibiting the release of free fatty acids and reducing blood brain barrier breakdown. Enhances cellular communication by increasing the availability of neurotransmitters, including acetylcholine, norepinephrine, and dopamine. Lowering increased glutamate concentrations and increasing the decreased ATP concentrations induced by ischemia. Citicoline increases dopamine receptor densities, and therefore could improve memory impairment resulting from poor environmental conditions. Citicoline could also improve focus and mental energy and could be useful in the treatment of attention deficit disorder. Citicoline has also been shown to improve visual function in patients with glaucoma [7].
Conclusion
The novel use of intramuscular cerebrolysin and citicoline in a patient with kernicterus was safe and effective.
Read More About Lupine Publishers Journal of Neurology and Brain Disorders Please Click on below Link: https://brain-disorders-lupine-publishers.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.