Lupine Publishers | Journal of Urology & Nephrology
Abstract
Objective: To describe step-by-step technique in Robot Assisted Radical Prostatectomy of our transperitoneal posterioranterior technique for prostatic dissection with preservation of the endopelvic fascia, preservation of the puboprostatic ligaments and dorsal venous complex.
Materials and Methods: Description of our surgical technique over 80 patients who underwent RARP and the characteristics group from 2016 to 2019 excluding the rest of cases who went to different surgical approach and technique for robot-assisted radical prostatectomy.
Results: The mean age was 63 years old, 7% of patients were overweight and 7.5% had obesity. The mean pre-operative prostate volume was 42.620 cc, mean prostatic specific antigen (PSA) of 10.414.8 ng/dl. The mean console time was 198±47. The surgical margins were positive in 13.75% of the patients. Complications were recorded in the peri-operative period, five (6.2%) Clavien-Dindo I and six (7.5%) Clavien-Dindo II.
Conclusions: After 8 years of experience in our center we have modified our technique of robot assisted radical prostatectomy, improving our results, following different worldwide concepts in the prostatic dissection. Even if necessary, to increase the number of cases we have find an easier way to reproduce with acceptable results.
Keywords: Robotic Radical Prostatectomy, Prostate Dissection, Transperitoneal Approach
Introduction
In the past year’s robot assisted laparoscopic surgery is
becoming more easily available in Latin America, in México
was introduce by our department in Mexico, City in 2013 we
accomplished the first robot assisted radical prostatectomy. At the
beginning we started performing an anterior technique, which is,
in most centers the standard of treatment for localized prostate
cancer.
The technique varies depending on the place of learning or
according to initial proctoring and preferences. Twenty years ago,
was introduced the laparoscopic approach, at that time was usual
the retrograde dissection starting with the apex. Guillonneau et
al., described the mixed technique modifying the Mountsouris
technique where they used and antegrade and retrograde
approaches in 7 standardized steps. [1]After in 2003 following several years of evolution in the robotic radical prostatectomy
technique the Frankfurt group published a case series of their
robot-assisted technique using ascending and descending
techniques for prostate approach [2]. In 2012 Asimakopuolus et al.,
described their intra fascial dissection of the neurovascular bundle
[3]. Several approaches since that time have been created.
In this article we describe our technique, which has been
modified since our initial experience from 2011, after learning the
lateral anterior approach in France, and then modifying to a mixed
technique in between anterior and the Bocciardi approach[4].
Materials and Methods
Description of our surgical technique over 80 patients who underwent RARP and the characteristics group from 2016 to 2019 excluding the rest of cases who went to different surgical approach and technique for robot-assisted radical prostatectomy at the same time.
Technique step-by-step
We include a single surgeon experience over 80 cases from January 2016 up to December 2019 of Robotic Assisted Radical Prostatectomy, following the next description of the technique.
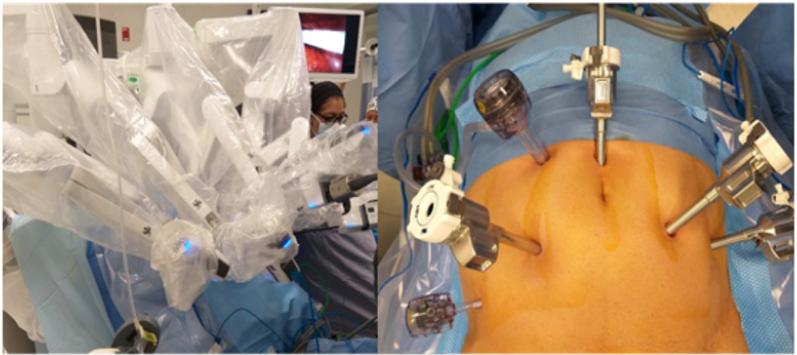
Port placement and Docking
The trocars placement starts once needle Veress insufflation of the cavity is performed. We use a four-arm X da Vinci robotic system (Intuitive Surgical, Sunnyvale, CA, USA). First robotic trocar is placed one centimeter higher to the umbilicus, two da Vinci X ports on the left side, first one, four cm to the left of the camera trocar and the second one, four more centimeters according to the anterior axillar line. On the right side, one more robotic port (8 mm) four centimeters from the camera port in a horizontal line. Two more accessory ports for the assistant are placed, one 12 mm port in a triangle between the camera port and first robotic port on the right, and a 5 mm port down and 3 centimeters upper the iliac crest (Figure 1).
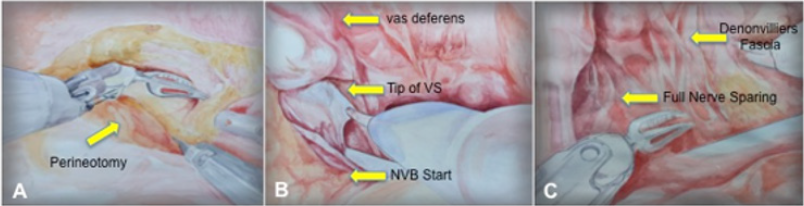
TransperitonealPosterior Dissection
Sigmoid dissection is performed to allow enough space in
the rectovesical area. Upper traction is done by the prograsp
instrument in the middle line in between bladder fatty tissue and
the line of the rectum. We follow the vas deferens reflection to start
the perineotomy through the pouch of Douglas.
Reaching the vas deferens we transected, we follow them
laterally for each side preparing the seminal vesicles, as the
description of Montsouris technique. The next step is to dissect
the full posterior base of the prostate, opening the Denonvilliers
fascia reaching the apex of the prostate area where the urethra
can be visualized, once we finish the medial space in between the
prostate and the rectum, we start the nerves bundles preservation.
By manipulating the right vesicle with the fourth arm, we expose
the angle of the vesicle tip and the base of the prostate.
The inferior and superior portions of the lateral face of the
prostate are dissected. Then we reproduce the same on the left
seminal vesicle, up traction to expose the base of the prostate and
we perform the nerve sparing on an antegrade way, if necessary we
place 5 mm clips coming from one of the assistant ports to avoid
the bleeding from the capsular arteries going through the prostate
and to control the prostatic pedicles. We can reproduce different
degrees of preservation, intrafascial, inter or extrafascial [5,6]
(Figure 2).
Once posterior base and lateral walls of the prostate are finished, we tract the seminal vesicles and perform a forward an up dissection in direction of the bladder neck, leaving the most anterior prostate bases (left and right) the closer to the start of the bladder neck, at this time we release the seminal vesicles and we move to the lymph node dissection, once accomplished the approach goes anteriorly.
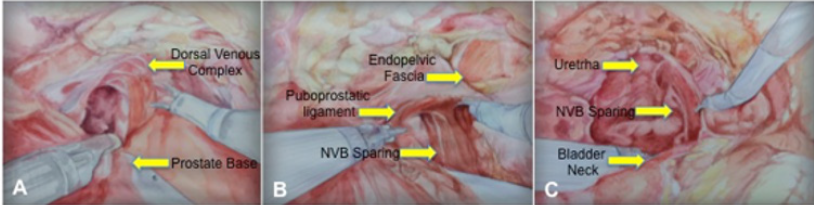
Transperitoneal Anterior Dissection
We go traditionally anteriorly to create the Retzius Space with
a parietal peritoneum incision, down the level of Cooper Ligament;
we identify all the anterior prostate suspension structures by
removing the fatty tissue that surrounds it. The bladder at this time
has been pull up by the forth arm, we perform and incision at the
lowest medial level of the puboprostatic ligament without opening
the endopelvic fascia but very near to the lateral prostate capsule,
we do respect the maximum length of the puboprostatic ligaments
[7].
The endopelvic fascia is preserved, we go laterally to the
prostate capsule from the initial incision up to the level of the
bladder neck anteriorly and laterally, because of the previous down
to up dissection and nerve sparing form the posterior dissection
we can easily visualized the nerves already spared. The same steps
are reproduced in the right side, sparing the endopelvic fascia, and
the maximum length of puboprostatic ligament, going down till the
bladder neck shape appears (Figure 3).
Once both sides accomplished, we do a close traction by the fourth arm Prograsp and decreased the bladder catheter balloon to 5 cc. A U inverted incision on the anterior wall of the bladder is done, a very spare bladder neck is accomplished by cutting the posterior bladder neck area, following deeper to a fully access to the previously dissected seminal vesicles, this step allows a very well neck sparing technique [8].
Lateral Prostate and Apex
Next step is to move the prostate lateral dissection toward the
apex, going close and down to the dorsal venous complex, without
cutting it or suturing it, we follow the angle going down to the level
of the urethra respecting the anatomical position of the plexus
over the urethra, the plexus stays at the level of the respected
puboprostatic ligaments and rounded endopelvic fascia.
We correctly identified the urethra diameter and transected
with the maximum length possible. The Denonvilliers fascia bellow
properly dissected avoids posterior reconstruction. For the urethral
– bladder anastomosis a van Velthoven technique is perform using
a 3-0 V-Loc [9]. Finally we use the same V-Loc suture from each side
of the anterior line of suture to recreate a suspension-like hammock
stitches; this is accomplished by using the end tip of the suture from
the lateral portion of the neck bladder to the previous position of
the puboprostatic ligament, with this we enhance hypothetically,
better continence. A Foley 18 fr catheter is placed with 15 cc inside,
finalizing the procedure. Prostate is removed through the camera
incision port.
Results and Discussion
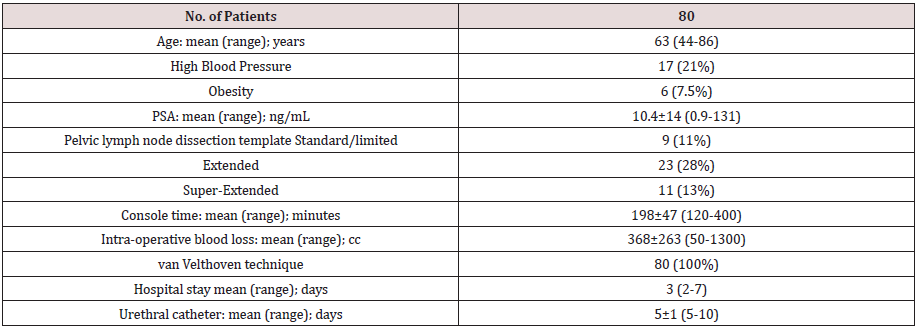
The patients were aged between 44 and 86 years old (mean:
63 years old). The most common co morbidity was high blood
pressure (n=17), seven percent of patients were overweight and
7.5% had obesity. The mean pre-operative prostate volume was
42.620 cc (range: 9.3-115), mean prostatic specific antigen (PSA)
of 10.414.8 ng/dL (range: 0.9-131) and mean positive cores per
biopsy were 4.93 (range: 1-12).
s
The mean console time was 19847 minutes (range 120-400)
and intraoperative blood loss was 368263 (range 50-1300). The
uretro-vesical anastomosis was performed with the van Velthoven
technique in 80 patients (100%). In 17 (21.3%) patients a closed
suction drainage was placed. [10] Five (6%) patients required
blood transfusion, and none required conversion to an open
approach [11] (Table 1). No major complications were recorded
in the peri-operative period, five (6.2%) Clavien-Dindo I and six
(7.5%) Clavien-Dindo II.
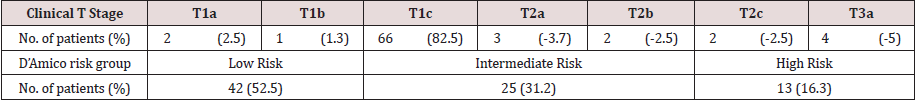
The RARP Gleason score were 6 in 36 (45%), 7 in 26 (32.5%), 8 in 7 (8.8%), 9 in 9 (11.3%) and 10 in 2 (2.5%) patients. The T clinical stage and D’Amico risk group is described in Table 2. Pelvic lymph node dissection was performed as follows: 9 (11%) standard/ obturator, 23 (28%) extended and 11 (13%) super extended.
The surgical margins were positive in 11 (13.75%) patients. The
most common positive surgical margin was at the level of prostatic
apex. [12]We found a positive Pearson correlation between RARP
Gleason score and positive surgical margins (r=0.539, p=0.01). The
mean hospital stay were 3 days (2-7 days), and the urethral catheter
was removed in a mean period of 51 day (5-10 days) [13,14].
Respecting, as other authors, the puboprostatatic ligaments
and the santorini complex as well as the endopevic fascia we can
spare much more the prostate fossa, avoiding too much invasion on
the pelvic structures. [15] Our final stich for an anterior suspension,
keeps part of the anatomy form the bladder to the ligaments. As
demostrated by Galfano et al., we bealive that starting the radical
prostatectomy through the pouch of Douglas is an easier way to
improve later during the procedure a most precise definition to the
bladder neck as also a better definition of the anterior anatomical
structures, and maybe is also a proper start if we want to fully
perform a robotic retzis sparing radical prostatectomy [16].
Conclusions
We decide after four years of performing transperitoneal
anterior dissection approach and base in different worldwide
leaders and techniques for robotic radical prostatectomy, that
some of the steps in the learning curve could be challenging, we
started posteiror dissection with good overall outcomes and a good
reproducible technique.
Due to hight evolution in the technique we decide to follow steps
to simplify the bladder neck approach. With posterior dissection,
we can reproduce, from the vesicle tip and going laterally up to the
body of the prostate a very fine neurovascular bundle dissection.
Going thought the Retzius space with the previous posterior
dissection gives a clear anatomical landmark to define a proper
bladder neck sparing and to approach the Santorini plexus from
behind and below avoiding anatomical damage and excessive blood
loss.
Different techniques have been described for robot assisted
radical prostatectomy, and the preference and expertise of surgeon
allows making different possibilities to the surgical robotic
approach.
Disclosure Statement
No competing financial interests exist.
Conflict of interest statement
All authors certify that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (e.g., employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Fundingsource
This work was not supported by any Foundation.
Competing Interests
Authors have no financial or non-financial competing interests to declare.
Authors’ Contributions
All authors have contributed equally to the drafting of the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgements
The authors declare that the development of the manuscript was not supported by an honorarium, a grant, or any other sources of support, including sponsorship or any material sources of support.
Read More about Lupine Publishers Journal of Urology & Nephrology Please Click on Below Link:
https://lupine-publishers-urology-nephrology.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.