Lupine Publishers| Journal of Cardiology Research & Reports
Abstract
Pulmonary valvular endocarditis is rare disease, the majority of reported cases previously showed isolated PV endocarditis without clear underlying predisposition factors. We report here a 52 ages female patient with endocarditis of pulmonary valve associated with sub valvular pulmonary aneurism, the underlying pulmonary valvular stenosis and RVOT stenosis were confirmed. The 2DTTE, 3D TEE and MDCT-640 were used to make exactly the diagnosis. Patient was under went an un complicated surgical procedure.
Keywords:Pulmonary valvular stenosis; TTE: Transthoracic Echocardiography; TEE: Transesophageal Echocardiography; RT- 3DTEE: Real-time-3DTEE; Endocarditis; Vegetation; MDCT: Multidetector Computed Tomography
Introduction
Pulmonary valvular stenosis is usually an isolated congenital anomaly and occurs in 7% to 12% of patients with congenital heart diseases [1]. and accounts for 80-90% of native outflow tract obstruction. Severe PS often associated with some degree of sub valvular stenosis resulting from RV hypertrophy. 3DTEE, MRI, Cardiac computed tomography can be used to better define the level of obstruction [2]. Bacterial endocarditis is a rare complication of the disease. Pulmonary stenosis with moderate to severe degree is stratified to intermediate to high risk of endocarditis [3].
Case Report
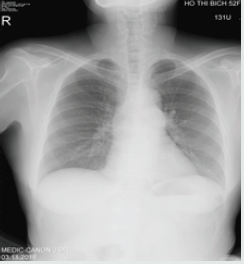
A female patient of 52 y.o presented at my hospital by persistent fever for one year, she had had this fever twice daily. Urine infection had been diagnosed and treated by Antibiotics in some hospitals, but the fever had been not interrupted. Finally, she came to MEDIC HCMC. Physical examination detected a 3/6 systolic murmur at the 3rd LICS like VSD. In her past history, no pathological finding has been noted. She was evaluated immediately by a chest X ray that demonstrated a slight prominence of the left second cardiac arch (Figures 1-4). The transthoracic echocardiography revealed a hypertrophic RV with normal TAPSE=20mm, normal LV size and function, EF=71%. Vegetation of 11x5mm in size that attached to the pulmonary valve, recorded from parasternal shorts axis view TTE.
The pulmonary cusps were doming and reduced opening degree, a severe pulmonary stenosis with max pressure Gradient=69mmhg, mean=42mmhg was confirmed by continue wave Doppler (Figures 5,6). Then Real-time 3DTEE was performed, and we found a mobile vegetation with greater size about 14x7mm associated with dilated pulmonary trunk of 35mm in diameter and a sub pulmonary valve aneurysm of 25x 36mm in measuring (Figure 7). CT angiography ( MDCT-640 ) with IV contrast medium Ultravist, slice thickness=0.5mm was indicated and detected a sub pulmonary valve aneurysm of 27x38mm and dilated pulmonary trunk: Annulus=27mm, Trunk=40-46mm, RPA=14mm, LPA=27mm. Furthermore, reduced RVOT size revealed: 9.5mm-10.2mm in diameter (Figure 8-11). Patient underwent uncomplicated surgical repair: opening RVOT, valvuloplasty and suture the perforated pulmonary cusp (this perforation was not seen prior to operation) with a favorable post-operative progress.

No comments:
Post a Comment
Note: only a member of this blog may post a comment.