Lupine Publishers | Journal of Pediatrics and Neonatology
Abstract
Background
In Burundi, maternal health care is mainly provided by midwives especially in peripheral health centres. However, midwives may not have needed knowledge and management capacity to offer care needed for women presenting maternal risks. This study assessed and modelled determinants of the knowledge and management of materno-foetal risk factors among midwives offering maternal health care in peripheral health centres in Burundi.
Subjects and Method
A cross-sectional survey was conducted on 90 midwives from 32 peripheral health centres offering maternal health care using a multistage random sampling. Dichotomous outcomes were built, and logistic models fitted on sociodemographic determinants. Significance of coefficients were detected using confidence intervals.
Results
Of 90 midwives, 57 (63%) and 63 (70%) had deficient knowledge level and management capacity of materno-foetal risk fectors; respectively. Younger midwives, those who studied in technical public schools, and those who had received professional trainings were more likely to have good knowledge. The effect of experience was inconclusive. Midwives whose work experience amounted up to 5 years were better off while those with higher experience accused having deficient knowledge. A good knowledge of maternofoetal risk factors predicted better management capacity up to seven times more (OR=7.21 [2.23-23.40]). Contrarily, male gender, long commute distance and the age above 45 years negatively predicted better management capacity.
Conclusion
In peripheral health centres offering maternal health care, newly recruited midwives and those who completed university education need further capacity building training to enhance both their knowledge level and management capacity related to materno-foetal risk factors.
Keywords:Midwives; Peripheral Health Centres; Materno-Foetal Risk Fectors; Knowledge Level; Management Capacity
Background
Majority of Burundian pregnant women consult peripheral health centres where the staff is mainly paramedical (midwives). Often, pregnant women present materno-foetal risk factors requiring special management (Poon, Mbonye, Bustan, Sheldon, et al. [1-4]). Therefore, knowledge of materno-foetal risk factors by midwives offering maternal care services (antenatal, childbirth, and postnatal care) is essential for risk management. In developing countries, commonly cited materno-foetal risk factors include chronic diseases such as diabetes, hypertension (HTA) and acquired immunodeficiency syndrome (AIDS); maternal and foetal history of pregnancy complications; as well as maternal factors such as extreme age (age<19 or age>35) and abnormal weight (BMI<19.5 kg/m2 or BMI>25 kg/m2) (Artal-Mittelmark, 2019). As per the World Health Organization (WHO) guidelines, most of these factors require specialised medical monitoring before and after childbirth (Organization, 2017, Carolan, 2009, Mamba, 2000). Therefore, midwives should be able to assess and grade maternal and foetal risk factors with an aim to transfer all women presenting one or more risk factor(s) requiring higher-level management. This study sought to shed more light on the level of knowledge and management of materno-foetal risk factors among midwives offering maternal health care in peripheral health centres in Burundi.
Subjects and Method
Study Design
We conducted a cross-sectional survey in 32 peripheral health centres in four health provinces namely Bururi, Cibitoke, Kayanza, and Rutana. The study was conducted on a period of two months, from April to May 2020.
Population and Sample
The study targeted midwives offering maternal health care in selected peripheral health centres. Selection of health centres was done using multistage sampling. In the first instance, four health provinces were randomly selected from a total of 18 health provinces. In each province, two health districts were randomly selected (n=8). In each district, four health centres offering maternal health care were randomly selected (n=32). The study was carried out on 90 midwives offering maternal health care.
We employed the following formulae to calculate the sample size:
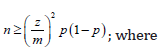
n = sample size
z = critical z score for α = 0.05
m = error rate (0.1)
p = prevalence of materno-foetal risk factors (p = 0.2)
Study Variables
We constructed two dependent variables; the knowledge level of materno-foetal risk factors and their management skills. The first outcome -level of knowledge of materno-foetal risk factors -was constructed based on a score from 26 knowledge questions; each question having a specific score scale. The overall score was reported as a percentage. The second outcome was the management capacity. It was constructed based on an overall score from 24 management questions. An average score was reported as a percentage. Indipendent variables included sociodemographic factors such as age, gender, civil status, education, professional experience, type of school attended, the number of professional trainings, and the commute distance.
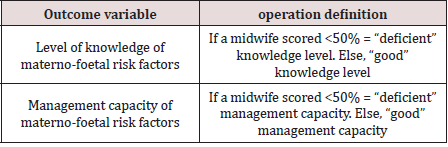
Operational Definition of Variables
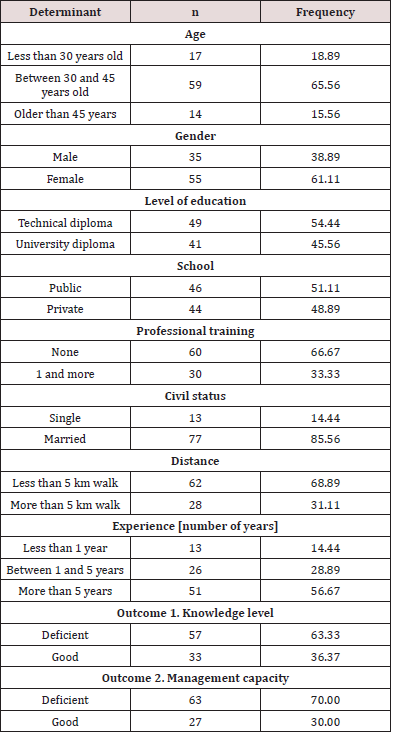
We constructed binary outcome variables coded “good” if a midwife achieved 50% or above, and “deficient”, otherwise. Details are presented in Table 1. Continuous independent variables such as age, number of professional trainings, number of years of professional experience, and the commute distance were categorized.
Study Instruments
All variables were obtained using a pre-established and tested questionnaire.
Data Analysis
Materno-foetal risk factors knowledge level
In the first instance, knowledge level was dichotomized, taking value 0 if midwife i scored less than 50%; and value 1, otherwise. Factors that determine the knowledge level were assessed using a logistic model. The model specification is as follows:
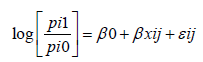
The dependent variable is the log odds that a midwife i scores j relative to alternative, where 0= deficient knowledge; and 1= good knowledge. Determinants are represented by a standard vector of covariates x. β0 captures fixed effects and β1 detect random effects on the probabilities of knowledge score.
Materno-foetal risk factors management capacity
In the second time, the management capacity was also dichotomised, taking value 0 if midwife i scored less than 50%; and value 1, otherwise. Factors that determine the management capacity were assessed using a logistic model as follows:
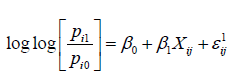
The dependent variable is the log odds that a midwife i scores j relative to alternative 0, where 0= deficient management capacity; and 1 = good management capacity. Determinants are represented by a standard vector of covariates x. β0 captures fixed effects and β1 detect random effects on the probabilities of management capacity score. In addition to standard covariates, the logistic model on the management capacity of materno-foetal risks included the level of knowledge as a predictor. To ascertain significance of coefficients in logistic models, we used confidence intervals – which the literature claims to be more reliable (Bewick et al. [5], Chakraborty et al. [6]).
Research Ethics
This study obtained a certificate of ethics issued by the Ethical Research Committee of the Faculty of Medicine, University of Burundi (Ethics Certificate no 03/04/2020). Informed consent were signed by each participant. The data collected were anonymous and confidential and exclusively used for purposes of the study.
Results
Sociodemographic Determinants
Sociodemographic characteristics of surveyed midwives are summarized in Table 2. 60% of midwives were middle-aged, female, and without professional training despite them having been working for more than 5 years. 86% of midwives were married and more than three thirds lived within five kilometers walk. There was no difference between the proportion of midwives who attended public versus private schools irrespective of the degree obtained. With respect to outcomes, 63% of midwives had a deficient knowledge level of materno-foetal risk factors and 70% had a deficient management capacity.
Logistic models
Materno-foetal risk factors knowledge level
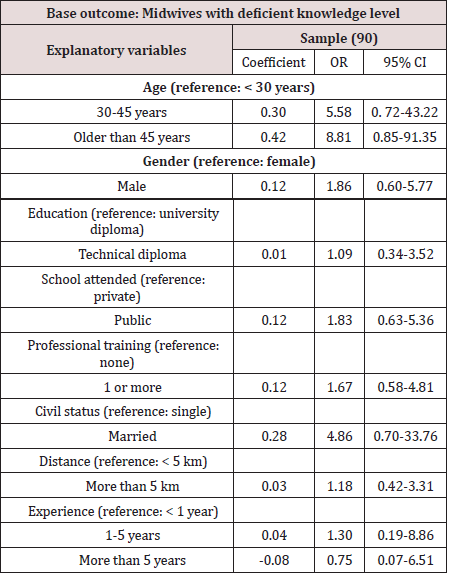
Table 3 summarizes results on the likelihood of a midwife
achieving a good knowledge score with reference to midwives
who scored deficient knowledge. In comparison with younger
midwives, the likelihood that a midwife scores good in maternofoetal
risk factors was more than five times for those aged above 30
years and again reached nine times more for midwives beyond the
age of 45 years. Being a male midwife who studied in a technical
public school was associated with a more likelihood of achieving
a good knowledge score (1
Materno-foetal risk factors management capacity
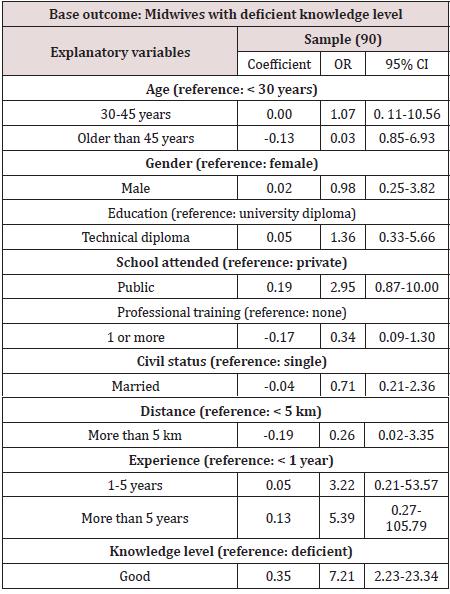
The model shows that midwives who had good knowledge of materno-foetal risk factors were more than seven times more likily to provide adequate maternal care when a woman presents with one or more risks (OR=7.21 [2.23-23.40]). Despite other coefficients being nonsignificant, the likelihood that a midwife provides better materno-foetal risk management was lower for midwives older than 45 years, for married or male midwives, as well as those who commute 5 km long to reach the workstation. Conversely, chances that a midwife performs better increased with the number of years of experience; reaching five times more for those who worked for more than 5 years. Also, in comparison with private school and university certificate, midwives from public and technical schools were more likely to offer better management of risk factors Table 4.
Discussion
This study, which targeted midwives offering maternal health care in peripheral health centres in Burundi, aimed to determine the level of knowledge of materno-foetal risk factors and further assess their management capacity. Results do not depart away from the existing literature. In the first instance, the likelihood that midwives have a better knowledge level related to materno-foetal risk factors was highly determined by older ages and married status. Also, male gender, technical degree, public school, professional trainings and the higher experience positively determined the better risk knowledge level. These trends have also been found in Ghana (Adams and Ray [7]), in Nigeria (Ashimi et al. [8]), and in other low- and middle-income countries. For instance, in a recent study which assessed determinants of the knowledge of maternofoetal risk factors among auxiliary midwives in Myanmar, older age and professional trainings were associated with more than twice higher knowledge level (Than et al. [9]). Tchounga et al. [10] in Côte d’Ivoire found similar results. In their study, better knowledge level of cervical cancer management of midwives was determined by exposure to professional trainings and the technical education (midwivery school) (Tchounga et al. [10]). However, our findings contradicted those in Tanzania where higher knowledge level was associated with younger ages (Urasa and Darj [11]). In our context, the decreased knowledge level among recent graduants could be ascertained to the decreasing quality of education which can be explained by the growing number of private and low-quality schools augmented by the lack of permant teachers (Obura, [12]).
With respect to materno-foetal risk management capacity, we
found an interesting positive contribution of the knowledge level. In
fact, midwives who have a good knowledge of risk factors are more
than seven times more likely to provide adequate care to mothers
presenting either risks. Other management enablers, though not
signicant, included higher work experience, professional trainings,
and training in public schools. In the study to determine factors
that affect midwives’ performance in pain management in Ghana,
inadequate professional trainings as well as being from a deficient
education background predicted poor performance (Aziato and
Adejumo [13]). Most importantly, in the same country, another
author established a strong correlation between the increased
number of years of experience and the higher likelihood of
providing better maternal and child health services (Jonas et al. [14]).
Midwives better performance was also cited in many other
studies including in Nigeria (Opiah et al. [15]), in Surakarta and
Karanganyar, Central Java (Wahidah et al. [16]), and in Omdurman
State, Sudan (Andugry et al. [17]). In our study, the likelihood of
better midwives’ performance predicted by the knowledge level of
risk factors (OR=7.21 [2.23-23.34]) is higher than most of evidence
in the literature. This trend could be associated with local context.
In our study, majority of midwives who scored higher knowledge
level of materno-foetal risk factors were mostly from ancient
technical education. Ideally, they constitute an excellent pool of
human resources in terms of health care provision [18-21].
We acknowledge the strengths and limitations of this study.
The study used a statistically significant sample and employed
multisampling techniques to minimise biases. This implies that
results can be generalised countrywide. A major weakness comes
from the study design. Despite cross-sectional designs generating
evidence on associations to guide policy, they do not allow causality
inference. Also, the study relied on self-reported data which can
fraught with Hawthorne effect. The contribution of this study is its
great policy implication. Results inform decision-makers and other
stakeholders on the need to strengthen the knowledge level and
management capacity of materno-foetal risk factors among most
of peripheral midwives. In conclusion, in peripheral health centres
offering maternal health care, newly recruited midwives and those
who completed university education need further capacity building
training to enhance both their knowledge level and management
capacity related to materno-foetal risk factors.
Financial Support and Sponsorship
This work was supported by the Medical Teaching Hospital of Kamenge.
Acknowledgement
We acknowledge all Health Province Officers and District Health Officers who have facilitated the conduct of this work.
Conflict of Interest
There are no conflicts of interest.
Read More About Lupine Publishers Journal of Pediatrics and Neonatology Please Click on Below Link: https://lupinepublishers-pedaitrics.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.