Abstract
Fractures of the femoral head associated with neck fracture and
posterior dislocation of the hip are uncommon. Pip kin and later
Brumback classified these complex fracture dislocations. However in
today's era patient have more atypical injury pattern. We encountered a
case which has never been described in literature and cannot be fit into
any previously described classification system. We present the
radiological details and management.
Introduction
Modern day accidents not only produce unpredictable but at times
unclassifiable injuries. Fractures of the femoral head associated with
posterior dislocation of the hip are uncommon as such [1]. Pip kin was
the one who sub classified Epstein-Thomas type V fracture-dislocations
into four additional subtypes which is still most widely followed [2].
Later Brumback et al. further classified femoral head fractures
emphasizing hip stability, with type "B" injuries being unstable [3].
The paucity of these cases is the main constraint to make an algorithm
of management. Nevertheless the results depend on early anatomical
reduction with the potential threat of osteonecrosis irrespective of
approach [4,5]. We hereby describe a case of posterior dislocation of
hip which is novel and never been described before. The purpose is to
make the fraternity aware of such a case which is unclassifiable even
though the management protocol may not be grossly different.
Case
A 52 year old migratory laborer had an accident at civil construction
site where he fell down from a height of 20 feet landing first on knees
(in kneeling position). He presented to emergency department with
severe pain in right groin, and inability to move the left lower limb.
On examination the limb was shortened, externally rotated and a bony
mass felt in the loin which did not move with the movement of distal
thigh. There was severe tingling and decreased sensation in front and
lateral aspect of leg and patient was unable to dorsiflex his ankle and
toes. His pulsations were normal but he had had transient hypotension
with tachycardia which corrected with initial resuscitation. First X ray
showed fracture about right hip (Figure 1) mostly a trochanteric
fracture but a careful evaluation showed incongruity of head and a
"vacant" on super lateral acetabulum. A CT scan was followed wherein the
fracture was better delineated. A posterior dislocation of hip with
fracture about the trochanter was seen. The head was also fractured and
the infra foveal part could be seen lying the acetabulum. A fracture
line also ran through the posterior wall of acetabulum which was not
more than 25% of the wall and also was undisplaced (Figure 2a- 2c). The
patient was admitted and limb placed in Thomas splint and prepared for
next morning. No attempts to reduce the dislocation were made.
Figure 1.
 Figure 2(a).
Figure 2(a).
 Figure 3(a).
Figure 3(a).
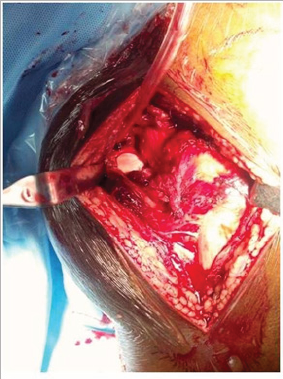
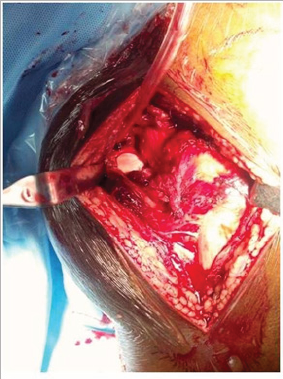
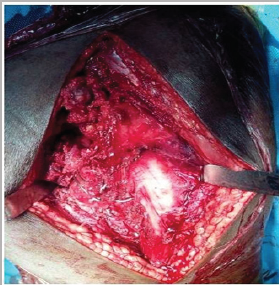
Under general anesthesia, the patient was positioned laterally and
a Moore's posterior approach was taken guided by dislocation and wall
fracture. The gluteus maximus had a huge rent and external rotators were
torn, the head was seen indenting the sciatic nerve (bowstring effect)
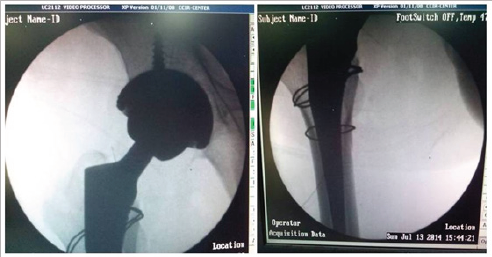
which was contused but intact (Figure 3a). The neck was ostetomised with
help of saw at the appropriate level and the calcar was reconstructed
using encirclage wiring (Figure 3b). Ethibond was used to suture the
greater trochanter. Next 2 temporary K wires were used in the ace
tabular walls and reaming done and cement less cup size 52 was fixed
augmented with 2 screws (Figure 3c). The K wires were removed after the
cup was found stable. The femur was prepared and uncemeneted corail stem
size 11 was inserted and size 36x0 femoral head was found stable. C arm
was used to confirm the placement of implants (Figure 3d). All soft
tissues were closed in best possible way, the hip was stable (Figure
3e). An abductor brace was applied post operatively. Postoperatively day
one faradic stimulation was started and patient was allowed side
tuning. Check X ray was done which showed a reasonable reconstruction
(Figure 4). The patient was allowed sitting with non weight bearing
mobilization from day 3 after the pain had subsided. 3 weeks after
surgery the patient was discharged when he went back to his home state
and never came back for follow up.
Figure 3(b).
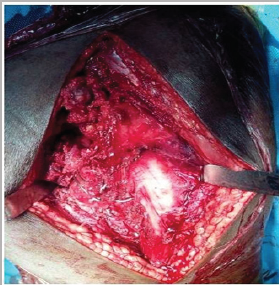 Figure 3(c).
Figure 3(c).
 Figure 3(d).
Figure 3(d).
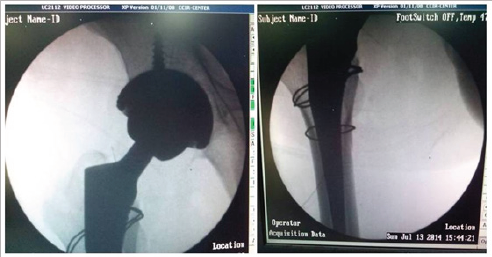 Figure 3(e).
Figure 3(e).
 Figure 4.
Figure 4.

Discussion
Femoral head fractures in combination with posterior dislocation of
the hip are rare presentation. Since first reported by Birkett in 1869
only a small number of cases have been reported world widen [6]. Epstein
et al.'s found about 10% in their series. It was Pip kin who subs
classified these fractures and various other classifications have been
proposed by several authors who claim to be improved version [5, 7].
Pipkin's classification remains most popular and widely accepted. They
divide them into 4 types with type 3 having associated ace tabular
fractures and type 4 having associated neck fractures. Our case is
unique with fracture in the trochanteric area. The trochanteric area has
never been described. The ace tabular fracture is also an addition
actually a combination pattern of Pipkin's 3 and 4. We believe that
there should be a type 5 including a both neck and ace tabular fracture
in association of head fracture and a subtype T wherein fracture
configuration is in trochanteric region instead of classical neck.
The cases of type 3 or 4 are very sporadic for any protocol to be
made. In younger individual attempts to fix the neck fragment, often
augmented with vascularised fibular graft has been made in past but long
term follow up is lacking. Osteonecrosis is a complication and surgeons
have tried different approaches with varying results [8,9]. In our case
closed reduction was not possible and moreover the impeding ischemia to
sciatic pushed.com for an early operative intervention. Taking into
consideration- a difficult fracture pattern, age, urgency of surgery,
peripheral set up hospital and an invincible avascular necrosis; we
thought a Total hip arthroplasty (THA) was an appropriate solution than
open reduction. Yet the challenges of choosing the right implant from
the whole Pandora box of prosthesis implants remained. In surgery, the
aim was to stick to principles of bone preservation like calcar
reconstruction and thus avoiding the distal fixation stems which were
reserved for future revision if a situation arose. A constrained hip
would have more advantages in this circumstance of soft tissue rent, but
the large head option of 36 was stable enough in our case. We admit
management to be debatable with expertise hands. Final outcome does
depend on return of sciatic function and proper occupational therapy
since he was a laborer. A draw back in our report remains that despite
best attempts to persuade the patient to visit nearest ortho clinic; he
never turned up but telephonically did tell to having a over the counter
sitting job in the village and satisfied with his hip.
Conclusion
The case highlights a rare injury and attempts to give an expansion
to the present Pipkin’s classification. Even though the demerit of this
report is a lacking follow up X ray and clinical picture, the initial
presentation is worth to be noted among the practioners and scholars.





No comments:
Post a Comment
Note: only a member of this blog may post a comment.