Lupine Publishers | Open access journal of Complementary and Alternative Medicine
Abstract
Keywords: Yin-Yang; The Five Element; Logic Thinking; Pattern Identification
Abstract
Both Traditional Chinese medicine (TCM) and acupuncture
originated in ancient China and has evolved for more than two
thousand years. However, most of the people generally in Taiwan
present themselves to the medical doctors first when they are in
need of medical treatments. Part of this fact is because there are not
sufficient scientific researches to prove the efficacy and safety of
TCM, acupuncture, moxibustion, acupressure, cupping, Tui na, and
tai chi. In Asia, such as Taiwan, Korea, Japan, Hong Kong, etc., herbs,
acupuncture, moxibustion, acupressure, cupping, Tui na, and tai chi
are often used by TCM practitioners to integrate mind and body to
treat or prevent health issues. Compared to the current TCM and
acupuncture developments in Taiwan, acupuncture and TCM have
gained more and more popularity in the past 40 years and been
considered “essential health benefits” by people in the United States
and the West, seeing and using acupuncture and TCM primarily as
a complementary health approach [1]. TCM and acupuncture have
established its status in the health system in the West, though
they’re totally different from the Western medicine with the
philosophy, diagnosis approaches, and pattern identification for
treatment. Challenges exist at present, which deserves attention for
those who are determined to learn or interested in understanding
TCM and acupuncture. This paper, therefore, tries to present some
issues for the better future of TCM, including acupuncture, and the
Western medicine when there are integrated.
Fundamental Differences between TCM and West Medicine
TCM, including acupuncture, and Western Medicine have been viewed as two distinct and divergent medicines for long with the approaches to physiology and healing techniques. Therefore, the fundamental differences in both Western medicine and TCM deserve attention when healthcare providers are considering the feasible choices in clinical practice to patients [1].In Theory
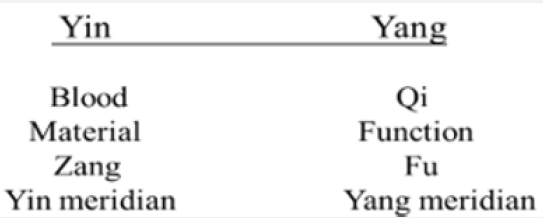
The philosophical concepts like Yin-Yang, the Five Element, pattern identification, and Qi and Blood are, to a certain extent, unique and abstract for learners to catch the whole picture with the functions broader than the anatomical knowledge in the Western medicine and are absolutely different from the theories of the Western medicine. In terms of relation of the human beings and the Heaven that can interact with each other in providing solutions to the health, it is totally different from the Western medicine that TCM sees the human body as a whole and as a microcosm of the universe in diagnosis and treatment, bringing the body, mind and spirit into harmony with Yin-Yang balance. It is believed that the concept of Yin-Yang balance is the unique concept indicating the harmony of internal organs and the dominating key of the TCM, which has served as the foundation and the guideline for the explanation of etiology of diseases, diagnosis, and treatments throughout the history of Chinese medicine and absolutely distinguishes TCM from the Western medicine [1]. Based on this concept, a disease thus refers to the loss of the balance of Yin-Yang [2].On the other hand, TCM focuses on the “congenital constitution” of the body that can result in “root” problems in health, which can scientifically correspond to the core thesis of Precision medicine (PM), which proposes the customization of healthcare with medical decisions, treatments, practices, or products tailored to the individual patient’s genetic content. In TCM, constitutions of humans are categorized into the five patterns for understanding the “root” causes and predicting the health conditions in the future, based on the Five Element theory [1]. Western medicine is seeking the minor difference from the perspective of etiology and only concerned about diagnosing and treating the symptoms alone. The theory develops with seeing the organs separately and treating parts of the body like a machine. Each part of the organs has its function, and when a particular part fails, it needs the replacement or resection [1,3].
In Practice
Treatments by medical doctors directly target at the pathogen or etiology with the evidence by a large number of modern scientific instruments, such as blood, urine, and stool tests, X-rays, CT, and MRI, to check on the human body. In addition to history taking and physical examination, doctors do not make diagnosis until all evidence are collected. Without scientific instruments, TCM doctors or acupuncturists can only make diagnosis, based on symptoms related to the imbalance of Yin and Yang rather than diseases itself through analyzing a patient’s tongue, pulse, voice, and whole-body situation, including reaction, hair, and posture [1,3]. The most important key to the successful results is that an experienced TCM doctors and acupuncturists can only rely on four skills for diagnosis to identify the patterns and write up the prescriptions. In other words, patterns, which distinguish TCM from the Western medicine, should be the key concern for the TCM and acupuncture practitioners in making the decisions of treatments. Since diseases are understood to be a loss of balance between Yin and Yang as shown in Figure 1, good results cannot be expected without the positive consideration of Yin and Yang [2,4].Challenging Issues
Language
There is no doubt that cultural decoding relies mostly on words. It is strongly accepted that “word-for-word” literal translation method is the way paraphrasing the accurate lexical meaning. However, this cannot be applied to TCM and acupuncture. Language is therefore the most challenging issue that needs to be addressed first. With the popularity of TCM and acupuncture, language barrier surely needs learners’ attention. The fact in the West currently is that not all of the TCM and acupuncture classics are translated into English. On the other hand, correct translation requires good translators excellent in both Chinese and English. In addition to the good command of these two languages, the meanings of the characters used in the ancient time may be different from those at the present time, which may confuse and frustrate readers. Chinese characters, different from alphabet languages which only represent forms and sounds, are called ideographs with three features of forms, sounds and meanings [5]. The difficulties in understanding Chinese characters in the TCM and acupuncture classics can be classified in the following ways [5]:A. Simplified Chinese is widely used all over the world; however, traditional Chinese is accepted and used in ancient classics and areas like Taiwan, Hong Kong, and Macao. For example, 黃帝內“經” in simplified Chinese is 黄帝内“经” in writing.
B. Pronunciation changed with usage. “能” is correctly pronounced neng in the modern Chinese, referring to “can” in English and. However, this character in Huang Di Nei Jing ( 黃帝內經, Yellow Emperor’s Inner Classic) means “state (態)” and the pronunciation is tai. This condition occurs when the characters were not enough for use in the ancient time.
C. “內” can be used either as a verb or a noun. It is pronounced na (equals納) when used as verb and nee when used as a noun referring to “inner” or “inside” in the modern use.
D. “平” is pronounced pin when it is related to an adjective “flat” in English. With writing mistakes, the pronunciation of this character is bian when it is used as a verb to mean “distinguish” in medical Chinese.
E. Different characters bear the identical meanings. “输”, “ 输”, and “腧” are different characters referring to the identical meaning of acupoint, and all of these three characters are pronounced shu.
The ability to understanding Chinese characters deserves attention as well in learning and understanding acupoints. For mastering acupuncture, understanding the real Chinese meanings of the acupoints is required. ST29-Guilai is the typical example for this aspect because Guilai (歸來) literally in Chinese means “return” and this acupoint is usually used for prolapse of uterus, menstrual irregularity, and dysmenorrhea [6]. 神(Shen) is translated differently into English in acupoints; for example, HT7-Shenmen ( 神門, Spirit gate) refers to the gate for Heart qi to get into and out of the body, while Heart governs Shen in TCM. Compared with the DU24-Shenting (神庭, Shen court), 門refers to gate in Chinese and 庭, court, which suggests that one must go through the “gate (HT7)” first and then get into the “court (DU24)” to hold or calm Shen. This difference highlights the importance of choosing acupoints in calming Shen. An acupoint may have different names with the historical developments. The nickname of KD3-Taixi (太溪) is呂細 (Lvxi) alternatively used in the acupuncture classics. On the other hand, the nickname of HT7 is 中都 (Zhongdu) completely identical with LV6 in Chinese, which may confuses learners.
Figure 2: Protocol matrix in using traditional acupoints
and extra acupoints.
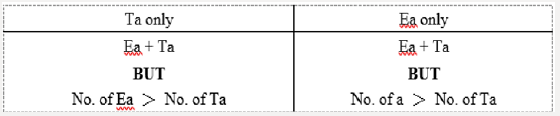
Note: Ea for Extra acupoints and Ta for Traditional
acupoints.
In addition to the names of acupoints, extra acupoints also
deserve close attention in consideration of combining regular
acupoints with extra acupoints. Extra acupoints distinguish
themselves from the regular acupoints on the traditional fourteen
meridians with the unique indications, actions, and the great
effectiveness in acupuncture theory and treatment, even though
some of extra acupoints have not been verified with scientific
evidence [7]. Pattern identification which derives from the Yin-
Yang theory is surely the key concept of TCM. Unfortunately, this
concept cannot apply to extra acupoints because they are not
incorporated into the traditional meridians with the lack of Yin-
Yang. The challenge acupuncture practitioners face is when it is the
best time to consider extra acupoints in a protocol. The historical
developments of extra points show that an extra point can surely
play an essential role in acupuncture and be used alone or with the
traditional regular acupoints for the treatment. Unfortunately, the
actions and indications of extra acupoints have not be scientifically
researched and verified as traditional regular acupoints. In
strategy, a practitioner may take the principle of “Least needling
for best results” into consideration to keep patients from pain, fear,
or worry. The goal can be achieved with the following four choices
shown in Figure 2 when it comes to the tactic [8].
Characterizations of Chinese Material Medica
The use of Chinese herb must be based on the patient’s conditions with accurate diagnosis, following the principles of pattern identification. Channels, properties, indications, and actions of the Chinese herbs in the different material medica classics are not always discussed in the same ways. The actions of Radix Ledebouriellae Divaricatae (Fangfeng) in Compendium of Materia Medica (Bencao Gangmu, 本草綱目), for example, are night sweat, migraine and headache, and constipation. However, actions like aversion to Wind, sweating, blurry vision, and vertigo are presented in The Classic of Herbal Medicine (Shennong Bencaojing, 神農本草經).Licorice root (Gancao, 甘草) with properties of sweet and neutral to tonify and strengthen the Spleen qi is effective for sore throat, bronchitis, cough, and infections caused by bacteria or viruses. This herb is the good example that highlights the time to collect herb is an attention that cannot be ignored. Literature shows the best time to collect and dry Licorice root is in the autumn two to three years after planting [9], but no detailed information is found for the reasons. The possible explanation for harvest time and cultivation time may be much to do with the compound differentiation, which can vary with moisture, temperature, and sunshine. The Chinese term 木瓜 (Mugua) refers to both Chinese herb Fructus Chaenomelis and papaya. In other words, confusing situation like this Chinese herb occurs quite often to TCM and acupuncture learners.
Processing
The nature and indications of Chinese herbs change with processing for the required actions in treatment.It is beyond doubt that Radix Bupleuri (RB) is one of the most popular traditional Chinese medical herbs in terms of treating diseases related to the Liver. Radix Bupleuri, named “Chaihu ( 柴胡)” in Chinese, is derived from the dried roots of Bupleurum Chinense DC. (Pei Chaihu, 北柴胡) and Bupleurum scorzonerifolium Willd (Nan Chaihu, 南柴胡) [10], which is the main ingredient of the most famous and frequently used preparations Xiao Chai Hu decoction and Da Chai Hu decoction. The major differences between Bupleurum Chinense DC. and Bupleurum Scorzonerifolium Willd are that the indication of Bupleurum Chinense DC. is dispersing stagnated Liver qi while Bupleurum scorzonerifolium Willd is raising Yang Qi in the Middle Jiao deficiency pattern.
For clinical use with indications changed to meet the patients’ needs, Radix Bupleuri is commonly selected in crude, fried, and vinegar-baked [11]. Among the characterizations of Chines herbs discussed above, dosage and ration are also two of the most important issues. Historic evolutions in the measurement show dosage, actually the top secret in learning Chinese formulas, has changed a lot and been a concern in practice for more than thousands of years. Quin (錢), the unique unit of weight measurement always used in TCM herbs, is different from that used in the Han dynasty, in which the author of Treatise on Cold Damage Disorders (The Shanghan Lun, 傷寒論) Zhang Zhongjing was born. In the meantime, one Quin equals 3.125g in China, but 4g in Taiwan, which suggests TCM and acupuncture learns need to bear the differences in mind when doing research. Another attention that should be given to the clinical use of Chinese herbs is dosage, which should draw attention with geographical factor. Zhang Zhongjing was born in Henan located in the south of China, where the temperate climate is humid subtropical. The climate may be one of the factors affecting his logic reasoning in the formulas; for example, the most used herbs in treating gastrointestinal diseases are licorice root, jujube, dried ginger, ginger, and Guizhi (Ramulus Cinnamomi) for the property of spicy to disperse stagnated Qi and tonify Yang. In other words, adjustments must be made, considering geographical factors.
In addition to weight, ration is also the concern that must been taken into consideration for the ingredient percentage of a formula. Liu Yi San (Six to One Powder, 六一散) indicates that the ratio of Talcum and Radix Glycyrrhizae (Licorice root) is 6:1. Actually, for learners who understand Chinese can easily catch the meaning of this formulas from the character 六 referring to six and-, 1. Dosages in practice must be adjusted, depending on the patients’ conditions. This is the most difficult to learn and understand because it reflects the experience of a TCM doctor or an acupuncturist. In other words, there is not golden rule to follow at all, and it is hard to be verified with quantitative analysis.
Discussion
Conclusion
https://lupinepublishers.com/complementary-alternative-medicine-journal/pdf/OAJCAM.MS.ID.000103.pdf
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
No comments:
Post a Comment
Note: only a member of this blog may post a comment.