Lupine Publishers | Journal of Gynaecology
Abstract
We report a case of 31 year old nulligravida with multiple sub mucosal and intramural fibroid uteri which was managed by laparoscopic myomectomy. She was asymptomatic and was diagnosed with multiple fibroid uterus and primary infertility. She and her partner were evaluated completely for other causes of infertility and all investigations were normal. She was further evaluated with mapping of myomas on Magnetic resonance imaging and underwent laparoscopic removal of all 10 fibroids in the same sitting. In this case report, we highlight the advantage and the technical challenges in laparoscopic removal of multiple sub mucosal fibroids in the same sitting that overcomes the complications encountered during hysteroscopic removal of multiple fibroids.
Keywords: Laparoscopic myomectomy; Infertility; Sub mucous fibroids; Multiple fibroids
Etiology & Pathogenesis
Fibroids are the most common benign gynaecological tumour that affects reproductive aged women with a prevalence of 20- 50% among them [1]. In general, uterine myomas are found in 5% to 10% of women with infertility. In 1.0% to 2.4% of women with infertility, myomas are the only abnormal findings [2,3]. Submucous myomas account for 5.5 % to 10 % of all uterine myomas [4]. Submucous myoma can be symptomatic irrespective of their size. They cause menorrhagia that can lead to anemia, infertility [5,6]. The route of surgery employed depends on the size, number and location of fibroid. Hysteroscopic resection of the myoma is the gold standard in selected patients with sub mucous fibroids (type 0,1,2). However, in women with associated subserosal and intramural fibroids, multiple sub mucosal fibroids with deep intramural extension(type1-5,2-5), sub mucosal fibroids more than 5 cm in size, laparoscopic route is the appropriate choice [7,8].
Hysteroscopic myomectomy has its associated complications of uterine perforation, fluid overload, uterine bleeding if performed by an inexperienced surgeon. Prolonged hysteroscopic surgery can lead to fluid overload and consequent electrolyte imbalance. In general, sub mucous myomas up to 4 to 5 cm can be resected hysteroscopically by an experienced surgeon but women with larger myomas and multiple myomas (>2 in number) benefit from laparoscopic surgery [8].
Case Report
We report a 31year old nulligravida who presented to.com with a diagnosis of multiple fibroid uterus when she was being evaluated for primary infertility. She has been married for 2 years. Her menstrual history is regular with no complaints of menorrhagia or dysmenorrhoea. She is a known hypothyroid on supplementation with thyroxin 25 mcg. No history of other associated medical co morbidities. There was no history of previous surgery. On clinical examination, the uterus was of 22 weeks size, irregularly enlarged, fibroid was palpable in right lateral, posterior fornices with restricted mobility. She was further evaluated with a Magnetic resonance imaging (MRI) mapping of the myomas which was suggestive of multiple fibroids, 10 in total. Five sub mucosal fibroids, two fibroids were intramural in location and three of them were subserosal. Both the ovaries were normal on MRI.
a. Operative Technique
The patient was operated under general anaesthesia in the modified lithotomic position. In view of multiple fibroids, five sub mucosal, two intramural and three subserosal in location the patient was planned for laparoscopic myomectomy. Hysteroscopic resection is the gold standard in management of sub mucous fibroids. However, laparoscopy was the best choice in our patient due to the presence of multiple (five) sub mucosal fibroids with large subserosal and intramural fibroids. The need for multiple sittings, prolonged operative time, and fluid overload that is more likely after hysteroscopic myomectomy can be completely avoided when managed laparoscopically. The presence of associated pathology like endometriosis can be dealt with concurrently. On abdominal examination, the uterus was noted to be of 22 to 24 weeks size. Pneumoperitoneum was created with veress needle in epigastria followed by closed technique insertion of primary optical 10mm supraumbilical trocar. Following this, three 5 mm and one 7 mm accessory ports were inserted under vision. The first accessory port was placed in the left lateral upper quadrant and the second accessory port was placed in the right lateral upper quadrant. The third and the fourth accessory ports were placed in the right and left lower quadrants respectively (Figure 1).
Figure 1: Port placement for laparoscopic myomectomy.

Figure 2: Uterus with multiple fibroids.
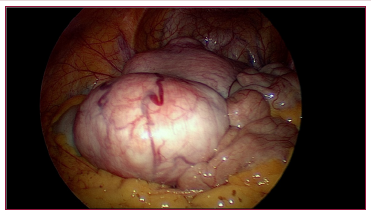
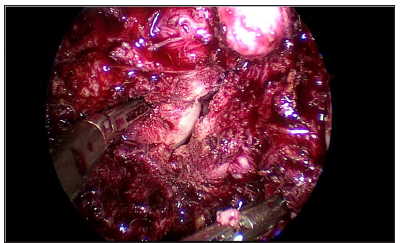
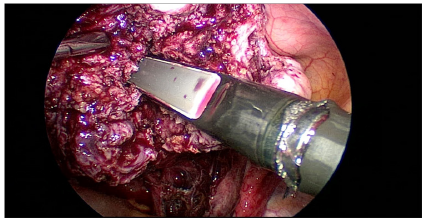
On inspection, uterus was studded with multiple fibroids and enlarged to 24 weeks size. 3 fibroids were visualised, the first one was a 6x4 cm subserosal fibroid of type 6 arising from the fundus, the second one was 3x 3 cm type 5 subserosal fibroid arising from the anterior and left lateral wall and the third one seen was a 2 x 2 cm subserosal type 5 fibroid arising from the anterior wall of the uterus lower body (Figure 2). Posteriorly, only the upper half of body of the uterus was visualised. Lower half of posterior uterine surface was densely adherent to the rectum and large bowel with both drawn up to 1/3rd body of the uterus. Rectum was separated from the posterior surface of uterus and while releasing the adhesions, chocolate material was drained. After releasing the bowel adhesions, entire posterior surface of the uterus was visualised. About 4x 4 cm intramural type 4 fibroid was seen in the posterior wall. Bilateral adnexa were normal. Bilateral uterine arteries were temporarily occluded with a hemostatic clip to minimise intraoperative blood loss that was released after the suturing of myoma bed (Figure 3). The posterior intramural fibroid was enucleated after giving a 5 cm vertical incision. Another 4x3 cm intramural fibroid type 4 was enucleated through the same incision. Through the same incision, the endometrial cavity was opened to 3 cm length (Figure 4). Five intracavitary sub mucous myomas were visualised, 2 sub mucous fibroids type 1, each measuring 2 x 2 cm, seen arising from fundus and posterior wall respectively. 3 sub mucous myomas type 2, each measuring 3 x 3 cm, 3x 2 cm, 2x2 cm were seen arising from the right lateral wall of endometrium.
Figure 3: Temporary occlusion of Uterine artery.
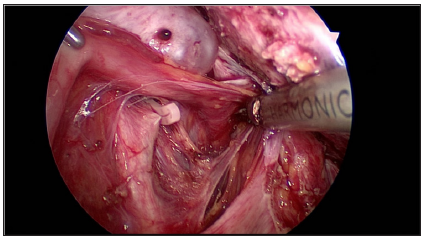
Figure 4: Opening the endometrial cavity.
All the above described fibroids were enucleated. Using laparoscopic endoultrasound, the entire uterus including the cavity was scanned intraoperatively to look for the presence of fibroids (Figure 5). There were no fibroids in endometrial cavity and uterine musculature as well. Myoma bed was sutured. The posterior vertical incision was closed in 4 layers. The endometrial cavity was sutured with No.3-0 PDS, the intramural layer was closed in 2 layers with V loc sutures and finally the uterine serosa was closed with No.2- 0 Vicryl. The 4cm transverse incision given to remove the fundal subserosal fibroid was closed in 3 layers with No. 2-0 Vicryl. The anterior 2 cm transverse incision for removal of the anterior lower segment fibroid was sutured with No.2-0 Vicryl in three layers. Uterine artery occlusion was released and hemostasis was ensured. The right lower port was converted to 12 mm and morcellator was introduced. Specimen was retrieved by morcellation in endobag.
Figure 5: sing an endoultrasound to identify the location of submucous fibroids.
Interceed adhesion barrier was kept over the suture line in the posterior wall, fundus and the lateral wall of the uterus. Abdominal drain of size No.20 was kept which was removed on the second postoperative day. Port closure was done for 12 mm and 10 mm ports with No.1-0 PDS. The estimated blood loss was 150 ml. The duration of the procedure was 3 hours from the time of veress insertion to suturing of skin. Skin was sutured with No.3-0 vicryl interrupted simple sutures. Post-operative recovery of the patient was normal. Urinary catheter was removed after 12 hours. She was started on liquid diet 6 hours after surgery. Intraperitoneal drain was removed on the second post-operative day as there was minimal drain output. Patient was given thromboprophylaxis for deep vein thrombosis with 0.6 ml low molecular weight heparin, 1 dose preoperatively and for 2 days post operatively. Her histopathology report was benign leiomyoma. The patient was doing well in her post-operative review. Postoperatively we have given the patient continuous oral contraceptive pills for 3 months to allow for endometrial healing. She is currently on follow up.
Discussion
Myomas have been known to impair fertility by several mechanisms including the creation of an abnormal site for placental implantation and growth resulting in infertility, an increased risk of spontaneous abortions, preterm labour and delivery [9]. The conception rate is approximately 53%–70% after myomectomy for sub mucous myomas, and 58%–65% after myomectomy with intramural or subserosal leiomyomas [10] Fibroids can be managed by laparotomy, laparoscopy and by hysteroscopic approach. The choice of surgery depends on the patient selection, skill and expertise of the surgeon. The laparoscopic route is employed for subserosal and intramural fibroids whereas hysteroscopy is recommended in the management of carefully selected patients with sub mucous fibroids [11]. There is a lot of debate on the management of sub mucous fibroids. Hysteroscopic resection of the sub mucous myoma has the advantage of avoiding an abdominal incision with faster recovery in well selected patients [11].
Sub mucous myomas (types 0, 1, and 2) up to 4 to 5 cm diameter can be removed under hysteroscopic guidance by experienced surgeons, whereas larger and multiple myomas are best removed abdominally. Type 2 myomas are more likely to require a multistage procedure than types 0 and 1 [8]. The main concern for the hysteroscopic surgeon being the risk of perforation especially when the myoma has a deep intramural component. Other possible complications include fluid overload, uterine bleeding and incomplete resection of the myoma. Prolonged duration of surgery during hysteroscopic resection of large or numerous submucous myomas can cause fluid overload and electrolyte imbalance. Traditionally hysteroscopic myomectomy was recommended in patients with the fibroid size smaller than 5 cm, < 50% of the endometrial surface is involved by myoma size or number, uterine size more than 16 weeks gestation or 10, 12 or 15 cm [11].
Amongst the numerous challenges that we had overcome in managing this case, the vital one was deciding on route of surgery. In our patient, we have managed the patient laparoscopically as the most likely reason for infertility in our patient was the presence of multiple sub mucous myomas(five). There was a high clinical suspicion of coexistent endometriosis. The presence of multiple fibroids involving more than half of the endometrium can cause endometrial damage due to use of energy sources (monopolar and bipolar) during hysteroscopic resection. Choosing hysteroscopic myoma resection in this patient will significantly prolong the duration of surgery and might result in inadvertent consequences. Laparoscopic myomectomy is preferable to the abdominal approach in many ways, in terms of rapid recovery, shorter hospitalization, reduced blood loss, fewer adhesion formation, simultaneous treatment of associated pathology and increased pregnancy rate. Nevertheless, laparoscopic myomectomy is a technically challenging procedure that requires surgical skill and expertise [8].
By choosing laparoscopic approach in this patient, we could enucleate all the myomas including the submucosal fibroids in the same sitting with minimal harm to the endometrium. Hysteroscopic myoma resection in our patient would require multiple sittings, significantly prolong the operative time and can cause increased endometrial damage as larger surface area of the endometrium would be lost during the removal of fibroid. We had performed temporary clamping of the bilateral uterine arteries with hemostatic clip that aided in significantly reducing the blood flow to the myometrium and hence minimized intraoperative blood loss during enucleation and facilitated quicker myoma bed suturing [12]. Permanent occlusion of the uterine vessels in women with leiomyoma associated infertility or the desire for conception must be judiciously employed. These women may have a greater risk of complications such as infection, chronic vaginal discharge, and spontaneous passage of an infarcted leiomyoma [8].
The biggest challenge we faced was planning the uterine incision. Based on the location of fibroids mapped in MRI and discussing with our team regarding the best approach to enucleate maximum fibroids with minimal incisions required, we had planned a posterior vertical incision. As majority of the fibroids on MRI were noted to be posterior to the endometrial cavity, they were easily approached by a posterior incision on the uterus. After enucleation of the intramural fibroids, the sub mucous fibroids were enucleated by opening the endometrial cavity. We had removed all the sub mucous fibroids through the same incision with the use of harmonic scalpel and location of the fibroids was accurately identified by laparoscopic ultrasound. This is a massive advantage in laparoscopic myomectomy as hysteroscopic myomectomy utilises monopolar and bipolar energy during myoma resection. The thermal damage to endometrium has been very minimal due to the use of harmonic in comparison to the use of monopolar or bipolar resectoscope [13]. Removal of five submucous myomas that are occupying more than 50 % endometrium by hysteroscopy may result in more endometrial damage.
The suturing of myoma bed is an integral component of laparoscopic myomectomy. The predominant concerns in the laparoscopic removal of a sub mucous fibroid are the risk of opening the endometrial cavity, healing of the suture line, formation of adhesions over the suture line especially in a posterior uterine incision, outcome of a subsequent pregnancy in a scarred uterus, risk of rupture in pregnancy following myomectomy [14]. Based on the clinical trials and case series, the risk of uterine rupture during pregnancy is no higher than 1% when the myometrial incision is appropriately repaired [15]. The suturing of myoma bed is difficult and technically demanding to achieve proper approximation and hemostasis. Our institute being a tertiary centre for advanced laparoscopic surgeries, the above technical challenges were efficiently managed.
Conclusion
Laparoscopic myomectomy is an effective procedure in patients with multiple sub mucosal fibroids associated with subserosal and intramural fibroids that are desirous of future childbearing as there will be lesser complications, minimal endometrial thermal injury and better chances of future conception. With the adequate equipment and technical skill, sub mucous myomas can be managed safely and effectively by laparoscopic surgery.
Acknowledgement
We thank the management and team of GEM Hospital and Research Institute for all the support and encouragement. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Read More About Lupine Publishers Journal of Gynaecology Please Click on Below Link:
https://lupinepublishers-gynecology.blogspot.com/
No comments:
Post a Comment
Note: only a member of this blog may post a comment.