Lupine Publishers| Journal of Diabetes and Obesity
Abstract
Obesity is currently considered to be the most common metabolic disease. During the last decades, its incidence has dramatically risen both in developed and developing countries. Several studies of the health of healthcare professionals have found that a significant proportion is obese. Obesity among the workforce may impede the efficacy of healthcare professionals health promotion efforts. The Mediterranean diet is considered to be a sustainable and healthy lifestyle pattern that promotes good health and disease prevention throughout the lifespan.
The objectives of the present study were
a) To determine the prevalence of obesity and obesity related lifestyle parameters (work anxiety, physical activity).
b) To investigate the association between adherence to Mediterranean diet and Body Mass Index (BMI) among health professionals.
c) To compare these parameters between medical doctors, administrative staff and nurses working at one selected public hospital. The perceptions of health professionals regarding their own body weight were also assessed and compared to their actual weight.
Keywords: Obesity; Health Care Professionals; Mediterranean Diet
Introduction
Worldwide obesity has nearly tripled since 1975. In 2016, more than 1.9 billion adults, 18 years and older, were overweight. Of these over 650 million were obese. According to the World Health Organization (WHO) (2017) overweight and obesity are defined as an abnormal or excessive fat accumulation that may impair health. Non communicable disease (cardiovascular diseases (mainly heart disease and stroke), diabetes, musculoskeletal disorders and some cancers) are linked to higher than normal BMI [1]. The Mediterranean diet, a sustainable and healthy lifestyle, represents the dietary pattern usually consumed among the populations bordering the Mediterranean Sea (one of them being Greece) [2]. The Mediterranean diet promotes good health and disease prevention throughout the lifespan. The notion of the Mediterranean diet has undergone a progressive evolution over the past 60 years since the first data from the seven countries study, from a healthy dietary pattern with increased adherence by populations living around the Mediterranean sea to a sustainable dietary pattern, in which nutrition, food, cultures, people, environment, all interact into a new model of a sustainable diet [3]. Several studies in different populations have established a beneficial role for the main components of the Mediterranean diet on the occurrence of cardiovascular diseases and non communicable diseases [4-6]. Adherence to a Mediterranean diet is associated with a significant improvement in health status, as seen by a significant reduction in overall mortality (9%) [7], mortality from cardiovascular diseases (9%), incidence of or mortality from cancer (6%), and incidence of Parkinson’s disease and Alzheimer’s disease (13%) [8,9].
Health professionals are considered role models for health for patients and their communities; nevertheless they face difficulties (e.g. night shifts, stressful working environment) in adhering to a healthy lifestyle, although they are aware of its benefits [10]. Health professionals educate, care, advice on healthy lifestyle, nevertheless epidemiological data show that they are in higher risk to have non communicable disease than the general population and that they do not incorporate in their everyday life important parameters of healthy lifestyle (e.g. physical activity, healthy eating) [11]. The aim of the present study was to investigate dietary habits and parameters of lifestyle of health professionals in a general hospital of Greece. The objectives of the present study were
a) To determine the prevalence of obesity and obesity related lifestyle parameters (work anxiety, physical activity).
b) To investigate the association between adherence to Mediterranean diet and Body Mass Index (BMI) among health professionals.
c) To compare these parameters between medical doctors, administrative staff and nurses working at one selected public hospital. The perceptions of health professionals regarding their own body weight were also assessed and compared to their actual weight.
Materials and Methods
This is a quantitative and cross-sectional study (n=150). Fifty medical doctors, 50 nurses and 50 administrative employees working at KAT public hospital were randomly selected. Data were collected by means of an ad-hoc questionnaire and anthropometric measurements. The ad-hoc questionnaire collected data on socio demographic characteristics of staff (gender, age, job category, and work experience), health status, health problems and risk behaviours, BMI and perceptions about body weight. Anthropometric measurements were recorded. Data collection was performed from November 2017 till December 2017. Worldwide overweight and obesity are estimated using the Body Mass Index (BMI) which is determined as a person’s weight (kg) divided by the square of his height (m) (kg/m2). According to WHO- a healthy BMI range is 18.5–24.9 kg/m2. Overweight is defined as a BMI from 25–29.9 kg/m2, and obesity is defined as BMI ≥ 30 kg/m2..
Adherence to the Med-diet was assessed by using the scoring methodology developed by Panagiotakos et al. [12] Eleven main components of the Mediterranean diet (non- refined cereals, fruits, vegetables, potatoes, legumes, olive oil, fish, red meat, poultry, full fat dairy products and alcohol) are assessed by MDS. For the consumption of items presumed to be close to this pattern the MDS assigns scores 0, 1, 2, 3, 4 and 5 when a participant reports no consumption, rare, frequent, very frequent, weekly and daily, respectively. For the consumption of foods presumed to be away from this pattern MDS assigns the scores on a reverse scale. Especially for alcohol, MDS assigns score 5 for consumption of less than 300 ml/day, score 0 for consumption of more than 700 ml/day or none and scores 1-4 for consumption of 300-400, 400-500, 500-600, and 600-700 ml/day (100 ml = 12 g ethanol), respectively. Then a total score ranging from 0 to 55 is calculated [13]. MDS predicts positive predictive values regarding hypertension, hypercholesterolemia, diabetes and obesity are: 45% (95% CI 43%-48%), 46% (95% CI 44%-49%), 12% (95% CI 11%-14%) and 33% (95% CI 30%-35%), while the negative predictive values are 86% (95% CI 85%-88%), 71% (95% CI 69%-74%), 98% (95% CI 97%-99%) and 97% (95% CI 96%-98%), respectively. Moreover, a 10- unit increase in the diet score is associated with 4% lower 10-year CHD risk (+/-0.1%, p<0.001) [14].
Work stress was measured with a 10-point Likert scale. Mean values and standard deviation (SD) were used for the description of quantitative variables. Absolute number (N) and percentages (%) were used for the description of qualitative variables. For the comparison of percentages, a Person chi square test was used. The analysis of variances was used in order to compare quantitative variables among three or more groups. For final interpretation of statistical significance, p = 0.05 was used. The SPSS 25.0 software was used for statistical analyses.
Results
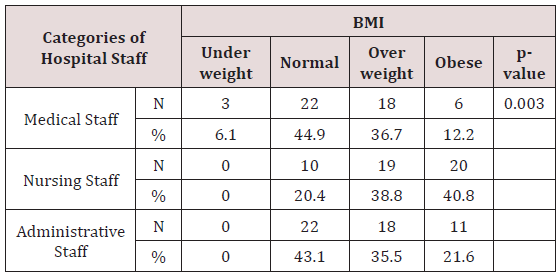
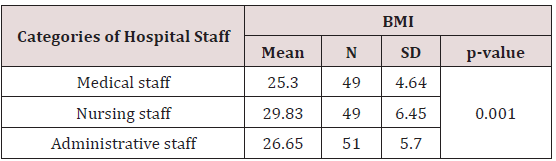
The majority of sample (59,1%) was female. The mean age was 44.7 (SD 9.7) and the mean of sedentary work was 3.8 (SD 3). Medical and administrative staff had 44,9% and 43,1% prevalence of normal weight, compared to nurses, who had 38,8% and 40,8% prevalence of obesity and overweight respectively (Table 1). A statistically significant difference was observed between prevalence of obesity and hospital staff (p=0.03). Body image was found to have statistically significant difference with BMI (p≤0.001) (Table 2). The majority of participants (55,3%) rated their working environment as stressful (Likert scale >7). No statistically significant difference was found between stress and different staff category (p = 0.711) and nor BMI (p = 0.875).
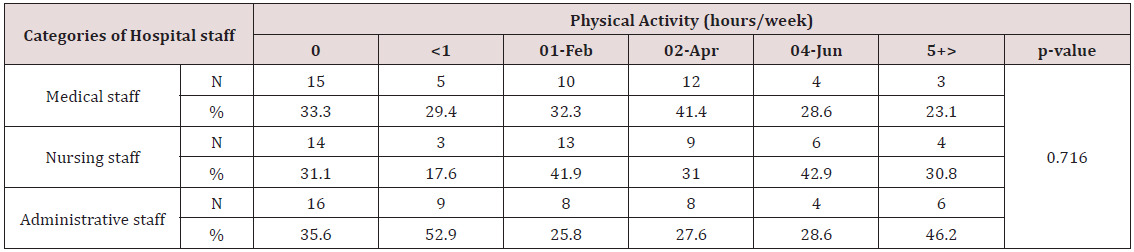
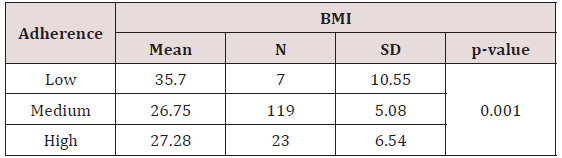
No statistical differences were found between job category and presence of cardio metabolic diseases (diabetes mellitus type 2, dyslipidemia, hypertension etc). As far as physical activity is concerned, 41,4% of medical staff walked 2-4 hours per week, 42,9%of nurses walked 4-6 hours per week, while 46.2% of administrative staff walked more than 6 hours per week. No statistical difference was found between physical activity and different participant group (p=0.716) (Table 3). The majority of participants (79.9%) adhered moderately to the Mediterranean dietary pattern, 15.4% high and the rest percentage (4.7%) low. No correlation was found between adherence to Mediterranean dietary pattern and different participant group (p=0.825). Participants with low adherence to Mediterranean dietary pattern had higher mean BMI (35.7kg/m2) compared with participants with moderate adherence to Mediterranean dietary pattern (26,75 kg/m2) and this difference was statistically significant (p=0.001) (Table 4).
Discussion
Health professionals educate, care, advice and investigate, but there are no particular programs to care for their health. Some authors have commented that nurses do not display ideal selfconcern about their health because they live a double sense of duty and are affected by their environment and job [15,16]. Although, they have enough self-care knowledge, they often do not have a correct self-care [17]. Health care employees, including nurses, are at increased risk on non-communicable diseases like diabetes, hypertension and coronary heart diseases. The main risks of NCDs are physical inactivity, poor dietary habits, smoking and alcohol abuse. NCD risk factors such as physical inactivity and adiposity based chronic disease have been widely reported among nurses in countries like Australia, United Kingdom, New Zealand and South Africa [10,18].
The findings about physical activity are in accordance with other studies which found that nurses do not meet the recommended levels of physical activity required for the benefit of health (30 minutes, 5 days a week). Our findings that emphasize the increased incidence of obesity in nurses are in accordance with till now research [10]. Healthy nutrition is α commonly used effective strategy to combat overweight and obesity, and as such has received considerable attention from the scientific community, either as a prevention measure or as an intervention strategy to fight overweight and obesity. Strategies to combat obesity and overweight nowadays focus on reducing total energy intake by portion control, nevertheless new scientific data on effective weight loss programs include as endpoints improvements on overall diet quality. Improvement of overall diet quality currently aims at adhering to diet patterns validated as healthy (e.g. DASH diet, Mediterranean diet, vegan diet) The Mediterranean healthy dietary pattern as a preventive and intervention strategy to manage excessive body weight has been extensively studied and used. Nevertheless the association between Mediterranean diet and obesity needs further investigation [3].
Exploring the relationship between the Mediterranean diet and overweight/ obesity is complex, and there are many methodological differences and limitations in the studies that make it difficult to compare results. Although the results are inconsistent, the evidence points towards a number of physiological mechanisms that can explain the possible role of the Mediterranean dietary pattern in preventing overweight/obesity [19]. The strongest association between obesity and Mediterranean diet was reported in the ATTICA study by Panagiotakos et al. [20] where individuals with a higher adherence to an MD were 51% less likely to be overweight/ obese. Our findings are also in accordance with a cross-sectional study by Park YM et al. [21] who analyzed data from 4700 adults aged 20–90, and concluded that comparing with the lowest MDS tertile, the highest tertile of MDS was associated with a 0.77 lower BMI (in kg/m2; P=0.004). There are several physiological pathways that could explain why key components of MD are beneficial for weight loss in obese patients [22] and for preventing excessive weight gain in healthy weight populations [23].
To begin with, the Mediterranean diet is mainly a vegan, yet not exclusively diet that consequently provide a large quantity of dietary fiber. This has been shown to increase satiety and satiation through mechanisms, such as prolonged mastication, increased gastric detention and enhanced release of cholecystokinin [24]. Energy density has an important role in weight gain, as palatable energy-dense food leads to poor appetite control and consequently to over-consumption. The Mediterranean diet is characterized by a low energy density and a low glycemic load compared too many other dietary patterns. These characteristics, together with its high water content, lead to increased satiation and a lower calorie intake, and thus help to prevent weight gain [19].
Another characteristic of the Mediterranean diet is the use of large amounts of olive oil. Taken into consideration that fat is more energy dense in comparison to carbohydrate and protein it would be expected that the Mediterranean diet that is a high fat diet would be associated with weight gain. However, there is some evidence that high fat diets are not the major cause of obesity, as important cohort studies and long-term trials have found no significant relation between higher fat diets and obesity. Contrary, the habitual use of olive oil (that is rich in monounsaturated fats) in salads and vegetables and legume dishes enhances palatability of these foods. This increases consumption of foods high in dietary fibre and low in energy density, resulting in greater satiation and satiety [19].
Moreover, the Mediterranean diet that is rich in monounsaturated fat has been found to improve glucose metabolism [25] and increase postprandial fat oxidation, diet-induced thermo genesis and overall daily energy expenditure compared with diets higher in saturated fats [26]. This may provide one more physiological explanation of why olive oil consumption is less likely to cause weight gain.
Finally, the Mediterranean diet is highly palatable and, therefore well liked and tolerated among dieters. As a result, compliance with the Mediterranean diet has been finding to be reasonably high [27]. Conclusively, the present study confirmed the till now research on increased prevalence of obesity among nurses comparatively with other health professionals. Stressful working environment and low level of physical activity did not contribute to a higher prevalence of obesity. The present study showed inverse relationship between adherence of the Mediterranean dietary pattern and prevalence of obesity in health care employees (medical doctors, administrative employees and nurses) working in a Greek public hospital. Taken into consideration the amputance of scientific evidence that associate Mediterranean dietary pattern with healthy weight, it is important that strategies to enhance adherence to Mediterranean diet of health professionals are adopted. Improvement of health professional’s overall health by combating obesity may improve their job performance and increase patient satisfaction out of health services provided. Overall, findings confirm the need for enhancement of adherence to a healthy lifestyle in health professionals.
Read More About Lupine Publishers Journal of Diabetes and Obesity Please Click on Below Link: https://diabetes-obesity-lupine-publishers.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.