Lupine Publishers| Journal of Otolaryngology
Abstract
Statement of The Problem
This provides an overview of Allergic Rhinitis and its management. It is very useful for students of Rhinology and clinicians managing this disease. It introduces them to a systematic approach of assessing allergic rhinitis patients which is very commonly found in most populations and causes considerably morbidity. Allergy per se is a very difficult subject to master and it is with great perseverance one can treat patients suffering from this condition. The cornerstone of managing a patient of allergic rhinitis is first and foremost obtaining a good history. This is to be followed by a thorough examination and investigations. The general practitioner is the first expert to be involved in management of allergic rhinitis patient followed by specialists otorhinolaryngologists, and finally by allied healthcare personnel. Inflammation of nose and paranasal sinuses are characterized by two or more symptoms-namely, either nasal blockage; obstruction; congestion or nasal discharge. Associated symptoms include facial pain; pressure and either reduction or loss of smell. Certain diagnostic endoscopic signs of nasal polyps and or mucopurulent discharge and or mucosal oedema in the middle meatus and or CT changes of mucosa within the ostoemeatal complex, and or sinuses are seen. Definitions, aetiologies, clinical presentations, diagnosis; prognosis and management of allergic rhinitis is dealt with. Common allergens causing the disease are mentioned, pathophysiology and classification of allergic rhinitis is discussed in detail. Different types of allergen testing are highlighted along with their specific role and uniqueness. Principles of immunotherapy in treatment of allergic rhinitis are discussed here. Health effects of allergic rhinitis along with its impact on physical quality of life is mentioned. The basic idea of this presentation is to improve diagnostic accuracy by promoting appropriate use of ancillary tests like nasoendoscopy, allergy testing, computed tomography etc. and reduce inappropriate antibiotic use. The basic treatment plan of allergic rhinitis is according to the severity and duration. It consists of allergen avoidance, pharmacotherapy, allergen immunotherapy and surgery which has limited role.
Keywords: Allergy; Rhinitis; Pollens; Molds; Insects; Penicillium; Cladosporium; Hypersensitivity; Histamine; Hay fever; Rose Fever; Transverse Nasal Crease; Rhinorrhea; Allergic Salute; Allergic Shiners (Dennie -Morgan Lines); Cobblestone Appearance Of Oropharynx; Scratch Test ; Intradermal Test; Patch Test; Rhinomanometry; Antihistaminics; Immunotherapy; Topical Nasal Steroids; Cochrane; Mast Cell Stabilizer
Abbreviations: IgA: Immunoglobulin A, IgE: Immunoglobulin E, AR: Allergic Rhinitis; NAR: Non-Allergic Rhinitis; ARIA: Allergic Rhinitis & its Impact on Asthma; Greater than; Less than; TM: Tympanic membrane; NPT: Nasal Provocation Test; n NO: Nitrogen in Nitric Oxide; PNS: Para Nasal Sinuses; OM: Occipito Mental; CECT: Contrast Enhanced Computerized Scan; L.A: Local Anaesthesia GA: General Anaesthesia; PQLI: Physical Quality of Life Index; WAO: World Allergy Organization; SCIT: Subcutaneous immunotherapy; SLIT: Sublingual immunotherapy; AIT: Allergic Immunotherapy; e-Health: Electronic Health; DBPC: Double Blind Placebo Controlled; RCT: Randomized Controlled Trial; FDA: Food & Drug Administration federal agency in USA; SMD: Submucous Diathermy; IT: Inferior turbinate; FESS: Functional Endoscopic Sinus Surgery; OMC: Osteo Meatal Complex
Introduction
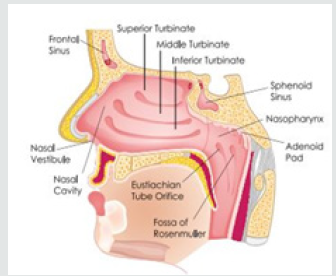
Rhinitis is a common presentation in E.N.T. clinics across the globe & allergy compounded with it causes even more difficult to treat for the clinician. This article is useful and handy for students and clinicians managing Allergy& Rhinitis. There is something in this for everyone-General Practitioners, Otorhinolaryngologists, Allergologists, Rhinologists and Allied Healthcare personnel. Special computer based newer modalities of investigations are highlighted in this which helps in assessing the nasal function of the affected patient. It’s very common to sometimes feel like sneezing & have running nose but please see a doctor if the feeling persists and do take care of yourself. Allergic Rhinitis is made so easy to comprehend. Nasal function includes temperature regulation, olfaction, humidification, filtration and protection [1]. Nasal lining contains secretion of IgA, proteins and enzymes. Nasal cilia propel the matter towards the natural ostia at frequency of 10-15 beats; min. Mucous moves at a rate of 2.5 -7.5ml. per min (Figure 1). Rhinitis is the presentation of two or more nasal symptoms for more than one a day namely Nasal congestion; obstruction, Rhinorrhea, Sneezing, Itching, Impairment of smell. Rhinitis occurs most commonly as Allergic Rhinitis. Non-infectious rhinitis has been classified as either Allergic or Non-Allergic Rhinitis. Allergic Rhinitis affects 15-30% of population with a wide geographic variance. It is more common in children & adolescents. 50% of all rhinitis in E.N.T. Clinics is Allergic Rhinitis. Allergic Rhinitis is defined as immunologic nasal response, primarily mediated by IgE. Non-Allergic Rhinitis is defined as rhinitis symptoms in the absence of identifiable allergy, structural abnormality or sinus disease. So, Allergic Rhinitis is an inflammation of the nasal mucosa, caused by allergen. It is the most common Atopic allergic reaction.
Aetiology
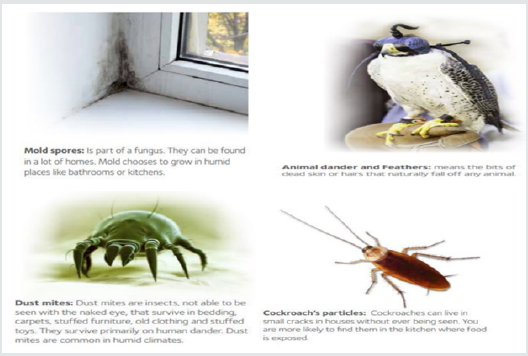
Aetiology is classified as Precipitating factors and Predisposing factors. Precipitating factors are classified into aerobiological flora and nasal physiology. Aerobiological flora are Allergens present in the environment, House dust & dust mites, Feathers, Tobacco smoke, Industrial Chemicals and Animal dander. Nasal physiology are Disturbances in normal nasal cycle. Predisposing factors are classified into genetic, endocrine, psychological, focal sensitivity tests, infections, physical, age & sex, IgA deficiency and common allergens [2]. Genetic factors indicate towards Multiple gene interactions are responsible for allergic phenotype. Chromosomes 5,6,11,12 & 14 control inflammatory process in atopy. 50% of AR pts. Have positive family history. Endocrine factors are Puberty, Pregnancy; Postpartum stages and Menopause. Infections such as Fungal. Physical factors are Degree of pollution of air, Humidity & Temperature differences, Temperature changes. Common allergens such as pollens (Spring tree pollens (Maple ; Alder ; Birch), Summer grass pollen (Blue grass, Sheep sorrel etc.), Autumn Weed pollen (Ragweed)), molds) Penicillium, Cladosporium etc.), INSECTS (Cockroaches, Houseflies, Fleas, Bedbugs) (Figure 2). Rhinitis is the presentation of two or more nasal symptoms for more than one a day namely Nasal congestion; obstruction, Rhinorrhea, Sneezing, Itching, Impairment of smell. Rhinitis occurs most commonly as Allergic Rhinitis. Non-infectious rhinitis has been classified as either Allergic or Non-Allergic Rhinitis. Allergic Rhinitis affects 15-30% of population with a wide geographic variance. It is more common in children & adolescents. 50% of all rhinitis in E.N.T. Clinics is Allergic Rhinitis [3]. Allergic Rhinitis is defined as immunologic nasal response, primarily mediated by IgE. Non-Allergic Rhinitis is defined as rhinitis symptoms in the absence of identifiable allergy, structural abnormality or sinus disease. So, Allergic Rhinitis is an inflammation of the nasal mucosa, caused by allergen. It is the most common Atopic allergic reaction.
Pathophysiology
Immunoglobulin IgE mediated type 1 hypersensitivity response to an antigen (allergen) in a genetically susceptible person. IgE is produced from plasma cells & the process is regulated by T-Suppressor lymphocytes or T-helper cells. IgE has affinity for mast cells & basophils and gets fixed to the surface of mast cells by its Fc end. Type 1 Hypersensitivity causes local vasodilation & increased capillary permeability. There is edema of the submucosal tissue by allergic fluid followed by infiltration by eosinophils and plasma cells leading to vascular dilatation which causes engorgement of the inferior turbinates and there is increased activity of seromucinous glands [4]. Histamine exerts its pharmacologic effect on smooth muscle, vascular endothelium & mucous glands. Number of IgE molecules has been estimated as 5300 to 27,000 in non-allergic subject & 15,000 to 41,000 in allergic subjects. Hypersensitivity of the host depends on antigen dose, frequency of exposure, genetic make-up, and hormone activity of the body.
Classification
Allergic Rhinitis is currently classified into intermittent and persistent. In intermittent AR the symptoms are present less than 4 days per week and less than 4 weeks per year [5]. In persistent AR the symptoms are present for greater than 4 days per week and for greater than 4 weeks per year. The severity of AR is classified into mild and moderate to severe. Mild AR doesn’t interfere with daily activities or doesn’t produce any troublesome symptoms. Moderate to severe AR interferes at least with one of the factors such as impaired sleep, hampered daily activities/work, school/ sick absenteeism, also produces troublesome symptoms. AR is formerly classified into seasonal and perennial based on the allergens. Seasonal Hay Fever, misnomer- no hay/no fever. Summer Cold caused by viruses causing URTI. Rose Fever seen usually in Indian Subcontinent (colorful/fragrant flowering plants). Perennial Allergens present throughout the year.

No comments:
Post a Comment
Note: only a member of this blog may post a comment.