Lupine Publishers | Journal of Anesthesia & Pain Medicine
Abstract
Background: Arrhythmias are one of the most serious disorders in cardiovascular and clinical medicine. Understanding the pathogenesis and mechanisms of arrhythmias is very advantageous to the appropriate management and treatment of all arrhythmia types. The “Graded phenomenon” is a novel directory phenomenon for understanding the arrhythmia. The principal of “Graded phenomenon” is based on catching the graded changes in serial ECG tracings or even single one regarding the arrhythmias.
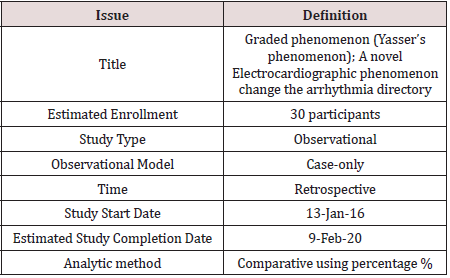
Method of study and patients: My case study was an observational retrospective for a 30 case report series. The study was conducted in both Fraskour Central Hospital (Intensive Care Unit, and emergency room) and Physician Outpatient Clinic. The author reported the 30-cases thorough nearly 4 years, started from Jan 13, 2016, and, ended on February 9, 2020.
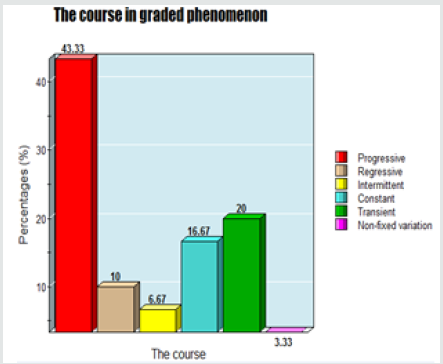
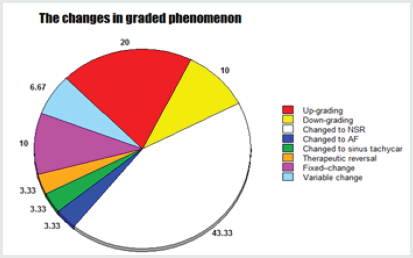
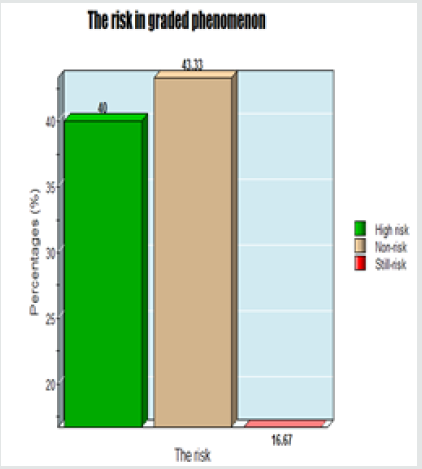
Results: The age mean is 58.3 years with male sex predominance (56.67%). The changes in graded phenomenon are classified into: Up-grading; 20%, down-graded; 10%, changed to NSR; 43.33%, changed to AF; 3.33%, changed to sinus tachycardia; 3.33%, therapeutic reversal; 3.33%, fixed –change; 10%, and variable change; 6.67%. The risk in the graded phenomenon is either high (40%), non-risk (43.33%), or still-risk (16.67%). The course in the graded phenomenon is either progressive (43.33%), regressive; 10%, intermittent; 6.67%, constant; 16.67%, transient; 20%, and non-fixed variation; 3.33%.
Conclusion: Graded phenomenon (Yasser’s phenomenon) is a novel electrocardiographic phenomenon change the arrhythmia directory. It is a crucial step for understanding arrhythmia. The phenomenon is a new strong guide for monitoring and follows up arrhythmic patients in cardiovascular patients.
Keywords: Graded phenomenon; Yasser’s phenomenon; A novel Electrocardiographic Phenomenon; Change the arrhythmia directory
Abbreviations: ABG: Arterial blood gases, AF: Atrial fibrillation, AMI: Acute myocardial infarction; ARVC: Arrhythmogenic right ventricular cardiomyopathy, BSOT: Bidirectional sectors of tachycardia, Congestive heart failure: CHF, CXR: Chest X-ray, ECG: Electrocardiograph, EADs: Early after-depolarizations, ED: Emergency Department, EPS: Electrophysiology studies, HR: Heart rate, HVS: Hyperventilation syndrome, ICU: Intensive care unit, IHD: ischemic heart disease, LVD: Left ventricular dysfunction, LVH: Left ventricular hypertrophy, MRI: magnetic resonance imaging, NSR Normal sinus rhythm, O2: Oxygen, PE: Pulmonary embolism, POC: Physician outpatient clinic, PVCs: Premature ventricular contractions, PVT: Polymorphic ventricular tachycardia, RA: Respiratory alkalosis, RBBB: Right bundle branch block, RBS: Random blood sugar, RR: Respiratory rate, SA Sinus arrhythmia, SAN: Sinus node, SCD: Sudden cardiac deaths, TdP: Torsades de pointes, VF Ventricular fibrillation, VT Ventricular tachycardia
Introduction
Arrhythmias
Scoping of arrhythmias: A heart arrhythmia is clearly described as a variation in the normal heart rate (HR) and/or rhythm regularity that is not physiologically justified [1]. Cardiac arrhythmias are happening if the electrical impulses that parallel your heartbeats don’t release precisely, causing tachycardia, bradycardia or irregularly [2]. Arrhythmia may be a serious problem especially if there are tachycardia or atrial fibrillation (AF) that can have serious consequences, including cardiac arrest and stroke [3]. Sudden cardiac death (SCD) is the cause of approximately 50 deaths due to cardiovascular disease (CVD) and nearly 15% of all mortality worldwide [4]. Almost 80% of SCD often due to ventricular arrhythmias [4]. Although most types of arrhythmia are benign, some will be predisposing to complications like stroke or heart failure [2]. Arrhythmias can kill 100,000 people in the UK annually [5].
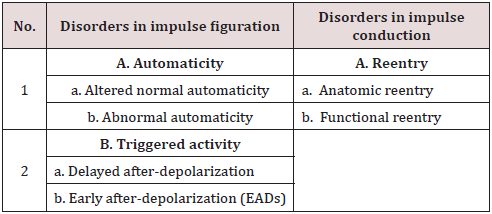
Mechanisms of arrhythmias: Understanding the mechanisms of arrhythmias is key to the appropriate management of all arrhythmia types 6. The mechanisms responsible for cardiac arrhythmias may be divided into disorders of impulse formation, disorders of impulse conduction or a combination of both6 Table 1. Modified from Gaztan L et al [6], Automaticity is the property of cardiac cells to generate spontaneous action potentials. Spontaneous activity is the result of diastolic depolarization caused by a net inward current during phase 4 of the action potential, which progressively brings the membrane potential to threshold [1]. Abnormal automaticity includes both reduced automaticity, which causes bradycardia, and increased automaticity, which causes tachycardia. Arrhythmias caused by abnormal automaticity can result from diverse mechanisms [1]. Early Afterdepolarizations (EADs) are typically observed in cardiac tissues exposed to injury, altered electrolytes, hypoxia, acidosis, catecholamines, and pharmacologic agents, including antiarrhythmic drugs. Ventricular hypertrophy and heart failure also predispose to the development of EADs [7]. EAD-induced triggered activity is sensitive to the stimulation rate. Antiarrhythmic drugs with class III action generally induce EAD activity at slow stimulation rates [8]. The ring model is the prototypical example of reentry around an anatomic obstacle [9]. In 1914, Garrey suggested that reentry could be initiated without the involvement of anatomic obstacles and that “natural rings are not essential for the maintenance of circus contractions [10].
Premature Ventricular Contractions (PVCs)
Premature ventricular contractions scoping: Generally, PVCs are the most common cardiac arrhythmia in patients with or without structural heart diseases (SHD) [11,12].
Premature ventricular contractions Pathophysiology: Premature ventricular contractions are early depolarization of the myocardium originating in the ventricle [13] caused by an electrical impulse or ectopic rhythm from any part of the ventricles, including the ventricular septum before the sinoatrial impulse has reached the ventricles [14]. PVC is a common arrhythmia triggered by impulses arising outside the normal conduction pathway of the heart that occur even in people with no underlying heart disease [15]. PVCs often arise from a pre-excitation, mostly in the right ventricle [11]. A PVC is a sign of decreased oxygenation to the myocardium but is also found in healthy heart [16]. In most cases, PVCs have a focal origin [17]. This means that an abnormal automatism, triggered activity or reentrant mechanism have an electric impulse of focal origin. This site of the impulse propagates centrifugally to the rest of the ventricles resulting in after depolarizations [12,18].
Premature ventricular contractions and the prognostic value: Currently, PVCs are considered progenitors of SCD [17]. Moreover, the studies revealed that PVCs were independent predictors of sudden and non-sudden death [19]. The concept that ventricular fibrillation (VF) and ventricular tachycardia (VT) are preceded by PVCs [17].
PVCs as a precursor for ventricular tachycardia and ventricular fibrillation: PVCs have also been shown to trigger malignant ventricular arrhythmias in certain patients with idiopathic ventricular fibrillation and persistent VT [18-20]. Persistent VT is very dangerous, as it can trigger ventricular fibrillation (VF) and SCD [14]. Patients with PVC couplets are more inducer for VT than with single PVC [21]. A higher PVC burden (> 26 %/day) is associated with left ventricular dysfunction (LVD), especially, in patients without SHD [22].
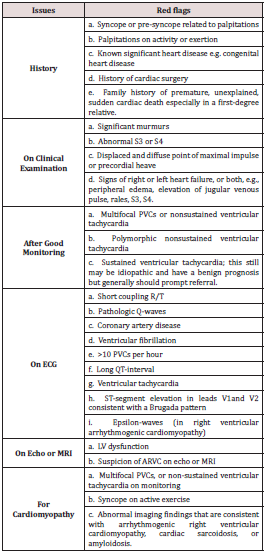
Prognosis and frequency and multiform of PVCs: The high frequent PVCs can vary from 10,000 to 20,000 PVCs/day according to relevant studies [23]. Frequent PVCs are associated with AMI and SCD in patients without known CAD24. Some studies carry a significant risk of AMI and SCD if there are >30 PVCs per hour [24-26]. Reports have suggested that frequent PVCs increase the risk of SCD, cardiovascular events, and LVD [27]. Multiform PVCs are associated with an adverse prognosis in the general population [28]. There are red flags and risk markers for premature ventricular contractions with a higher risk for SCD Table 2. ARVC: Arrhythmogenic right ventricular cardiomyopathy, MRI: magnetic resonance imaging, Modified from Elsayed et al [2].
Long-QT syndrome and polymorphic ventricular tachycardia (PVT): Torsades de pointes (TdP) is a specific form of polymorphic ventricular tachycardia (PVT) in patients with a long QT-interval. It is characterized by rapid, irregular QRScomplexes, which appear to be twisting around the ECG baseline. This arrhythmia may cease spontaneously or degenerate into ventricular fibrillation. It causes significant hemodynamic compromise and often death. Diagnosis is by ECG. Treatment is with IV magnesium, measures to shorten the QT-interval, and directcurrent defibrillation when ventricular fibrillation is precipitated [29-31].
Sinus Arrhythmia
Normal sinus rhythm: Normal sinus rhythm (NSR) is the rhythm that origins from the sinus node (SAN) and identify the known rhythm of the healthy heart [32]. The rate in NSR is commonly regular. But it varies depending on autonomic inputs into the SAN.
Sinus arrhythmia scoping: The term sinus arrhythmia refers to a normal phenomenon of alternating mild acceleration and slowing of the heart rate that occurs with breathing in and out respectively [33]. When there is an irregularity in the sinus rate, it is termed sinus arrhythmia (SA) [1]. Sinus arrhythmia is a common change in the NSR [34,35]. Sinus rhythm with a beat-to-beat variation in the P-P interval (the time between successive P waves), producing an irregular ventricular rate [36]. It is usually quite pronounced in children and steadily decreases with age. This can also be present during meditation breathing exercises that involve deep inhaling and breath holding patterns [37].
Sinus arrhythmia characteristics: Sinus arrhythmia characteristically presents with an irregular rate in which the variation in the R-R interval greater than 0.12 seconds34 or the P-P-interval of more than 120 ms (3 small boxes) [35-38]. There should be a 10% difference between the maximum and minimum cardiac cycle length [8]. The P-P interval gradually lengthens and shortens cyclically, usually corresponding to the phases of the respiratory cycle7 with normal sinus P-waves with both constant morphology [35, 36] and P-R interval [35, 36] Sinus arrhythmia is a physiological condition that most commonly occurs in the young healthy adults [34, 36] and children [34]. Sinus arrhythmia is a common incidental sign seen on routine Electrocardiogram (ECG) [34]. Often an asymptomatic and normal finding, the evaluation of sinus arrhythmia is limited. Generally, SA is at most mildly symptomatic (e.g., palpitations) [39].
Sinus arrhythmia prognostic value: Typically, its presence is a prognostic indicator for good cardiovascular health [34, 35]. Loss of SA may indicate underlying heart failure or structural heart disease [33].
Junctional Arrhythmias
Junctional arrhythmias nomenclature: The implicated nomenclature10 to recognize the type of junctional rhythms (JR) is based on their rate. They are classified as follows: 1. Junctional bradycardia: Ventricular rate ˂40 bpm [2]. Junction escape rhythm: Ventricular rate 40-60 bpm. 3. Accelerated junctional rhythm (AJR): Ventricular rate of 60-100 bpm. 4. Junctional tachycardia: Ventricular rate >100 bpm [40].
Junctional arrhythmias pathophysiology: If there is a blockage for the sinoatrial node (SAN) electrical activity is blocked or is less than the automaticity of the atrioventricular node (AVN)/ His Bundle a JR starts [41].
Junctional arrhythmias causative conditions: Numerous conditions and medications can lead to a diseased SAN and lead to the AVN/His Bundle to take over due to the higher automaticity of the ectopic pacemaker [42-44]. Hyperkalemia, sick sinus syndrome, pericarditis, myocarditis, unstable angina, acute myocardial infarction, repair of congenital heart disease, atrial septal defect, tetralogy of Fallot, persistent left superior vena cava, adenosine, digoxin, calcium channel blockers, lithium, amitriptyline, clonidine, reserpine, inhalation anesthetics, cimetidine, isoproterenol infusion, narcotics, beta-blockers, and ivabradine implicated in causing junctional tachycardia [41].
Paroxysmal Supraventricular Tachycardia
Paroxysmal supraventricular tachycardia scoping: Paroxysmal supraventricular tachycardia (PSVT) accounts for intermittent episodes of supraventricular tachycardia with sudden onset and termination. PSVT is part of the narrow QRS-complex tachycardias with a regular ventricular response in contrast to multifocal atrial tachycardia (MAT), atrial fibrillation (AF), and atrial flutter [45].
Paroxysmal supraventricular tachycardia scoping: PSVT is often due to different reentry circuits in the heart, where less frequent causes include enhanced or abnormal automaticity and triggered activity. Reentry circuits include a pathway within and around the SAN, within the atrial myocardium, within the AVN or an accessory (AP) pathway involving the AVN. Different types of PSVT result depending on the existing circuits, and examples are: a. SANN: Sinoatrial node reentrant tachycardia.
b. Atrial myocardium: Atrial flutter, AF, and MAT.
c. AVN: Atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT) [46-48].
Methods of Study and Patients
My study was an observational-retrospective study for 30-case
report series targeting the graded changes in arrhythmia using the
serial electrocardiography (ECG) tracings. Premature ventricular
contractions (PVCs), junctional arrhythmia, sinus arrhythmia,
paroxysmal supraventricular tachycardia, and atrial fibrillation
were the commonest goal in the study. The new phenomenon
“Graded phenomenon” is a constellation of the graded changes in
serial ECG tracings or even single one regarding the arrhythmic
patients. The author reported the 30-cases of thorough nearly
4 years, started from January 13, 2016, and, ended on February
9, 2020. The study was conducted in both Fraskour Central
Hospital (Intensive Care Unit, and emergency room) and Physician
Outpatient Clinic (POC) Table 3.
a. The changes in the cases of “Graded phenomenon” are
classified into:
1. Up-grading, 2. Down-grading, 3. Fixed change, 4.
Spontaneously changed to normal sinus rhythm, 5. Spontaneously
changed to another arrhythmia, 6. Therapeutic reversal.
b. The extension for arrhythmia in the cases of “Graded
phenomenon” are classified into:
• The up-grading phenomenon with the right to the left
extension
• The up-grading phenomenon with the left to the right
extension.
• Up-grading bidirectional sectors of tachycardia (BSOT).
• Intermittent Wandering pacing rhythm with the left to the
right extension.
c. The risk in arrhythmia in the cases of “Graded
phenomenon” are: 1. High, 2. Non-risk, 3. Still-risk.
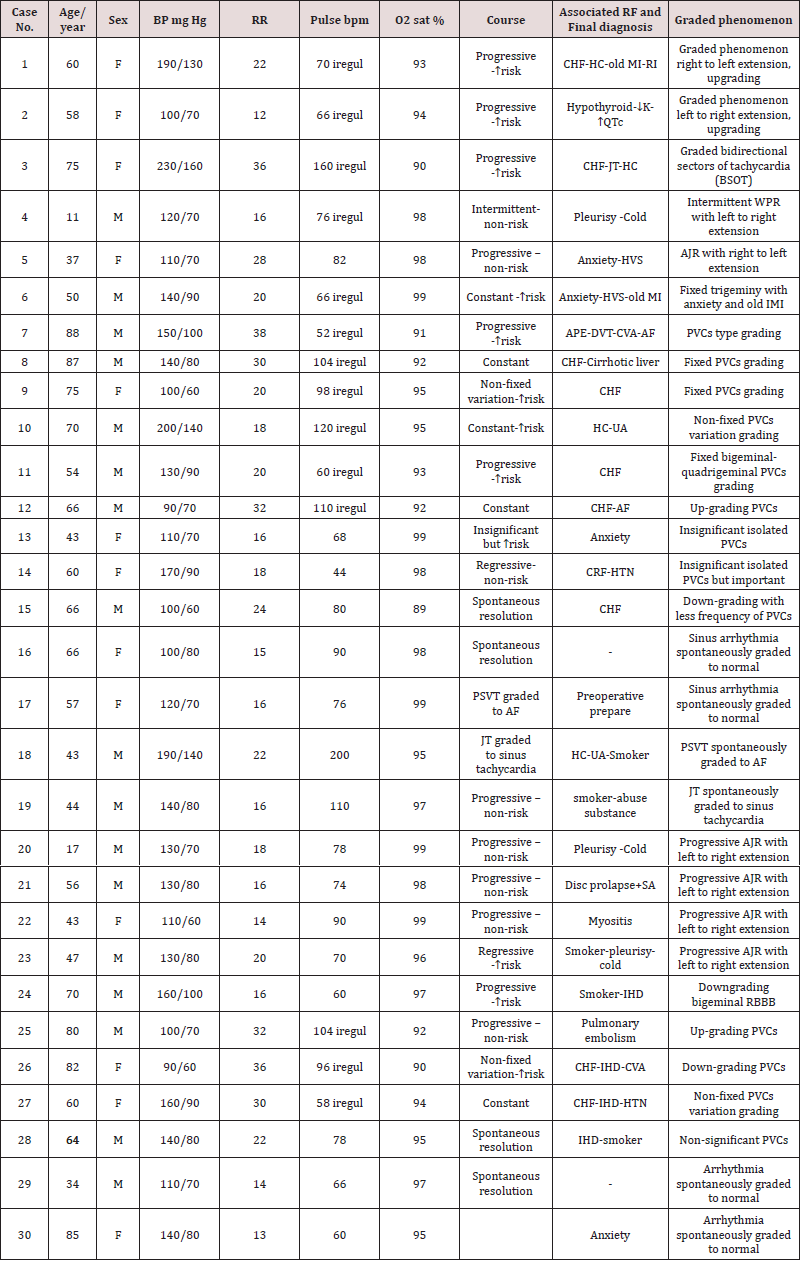
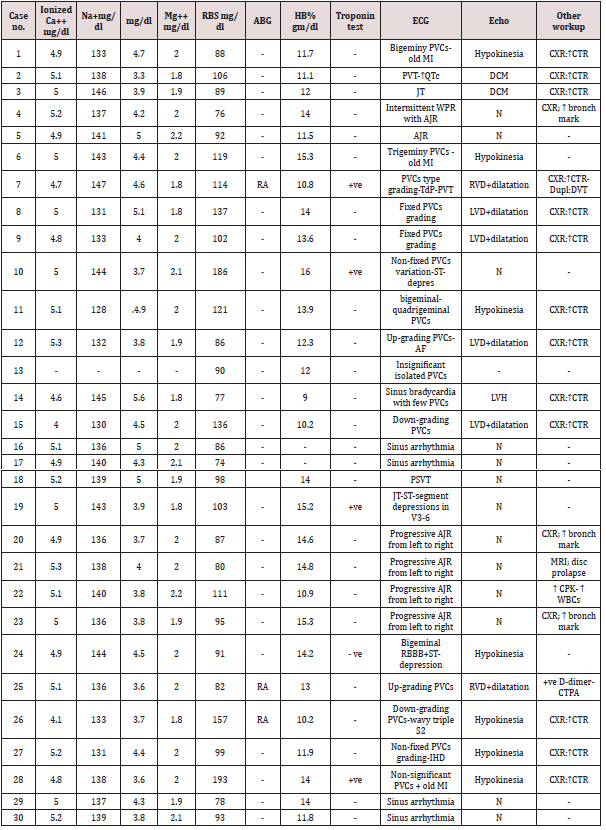
d. The principal of the “Graded phenomenon” (Yasser phenomenon) is based on catching the graded changes in serial ECG tracings or even single one regarding the arrhythmias. All cases were undergone to complete clinical examination and serial ECG tracings doing during follow up. Specific investigations were worked in the study. Serial ECG tracings, blood electrolytes (ionized calcium, sodium, potassium, and magnesium), complete blood counts, and random blood sugar nearly were done for all cases. Arterial blood gases, troponin test, d-dimmer, CPK-MB, echocardiography, helical thoracic computed tomography (TCT), and chest X-ray (CXR) were done in selected patients. Most of the cases were admitted to the ICU. Few cases were managed as clinic outpatients in POC with later follow up. Regards the remarks of the study method and data were summarized Table 3. For more details on general, clinical, and laboratory data for the cases see Tables 4-6. Table 3 showing remarks of the study method and data.
1. Eligibility criteria, 2. Inclusion criteria, 3. All cases of arrhythmias with graded electrocardiographic (ECG) changes especially; premature ventricular contractions (PVCs), junctional arrhythmia, and sinus arrhythmia. Patient ages ranged from 11 and up to 88 years old, 4. Exclusion criteria: Purely non-arrhythmic disorders, 5. Limitations of the study: There are no limitations to the study
Cases Presentation
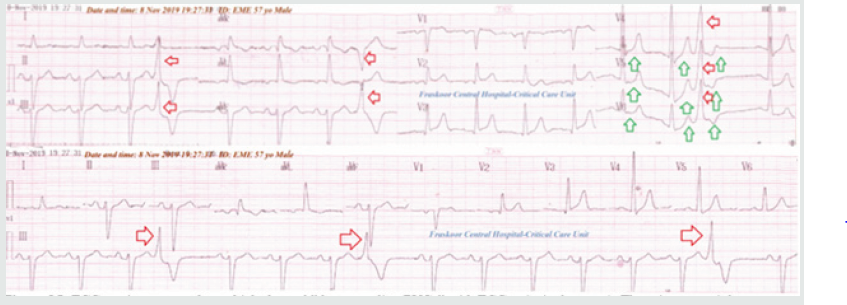
Case no. 1: (progressive Bigeminy Pvcs With Graded Phenomenon Right To Left Extension, Upgrading)
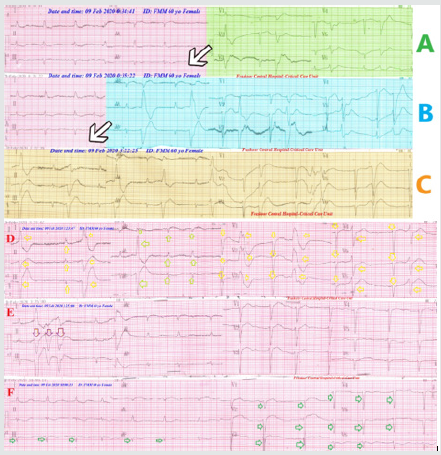
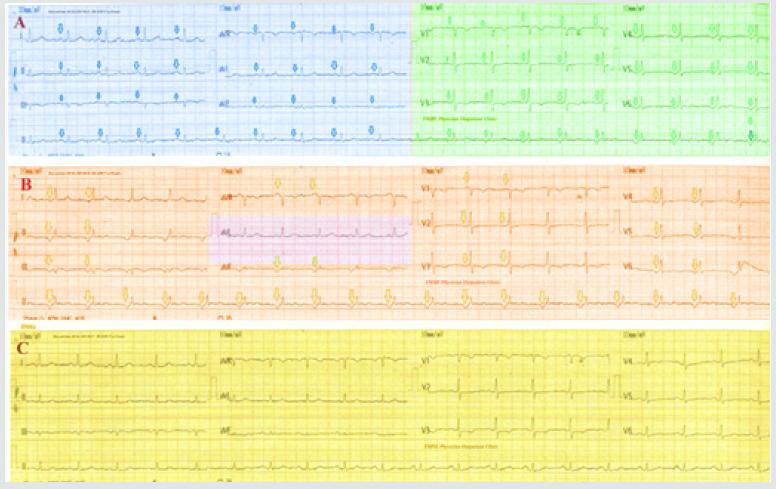
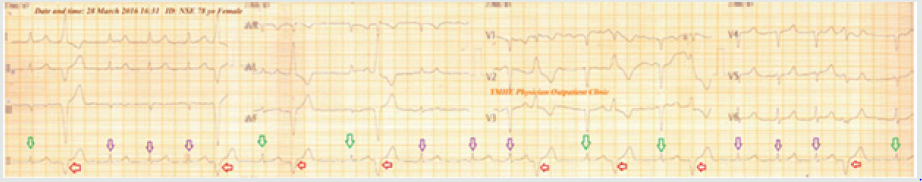
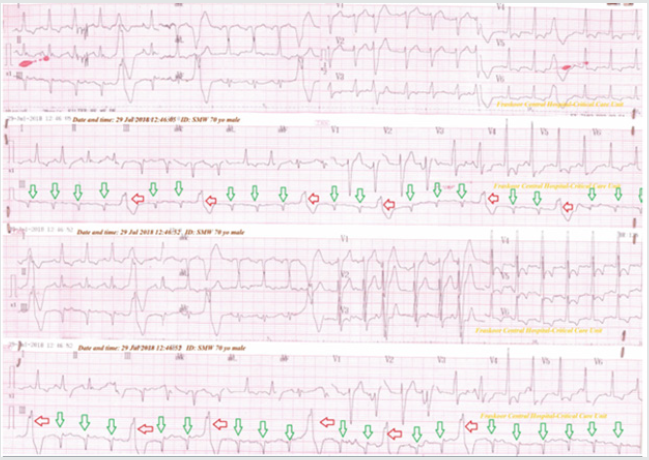
A 60-year-old married, housewife, Egyptian female, presented to the Emergency Room (ER) with orthopnea of progressive course. The patient admitted and managed in the intensive care unite (ICU) as chronic heart failure (CHF) with hypertensive crises (HC). She gave a history of diabetes and calcular cholecystitis. Clinically; the case manifested with heart failure. Serial ECG tracings were taken which showed an interesting progressive bigeminy PVCs was described as: “Graded phenomenon right to left extension, upgrading” (Figure 1). Bigeminy PVCs initially started in V1-6 leads (all chest leads) (Figure 1A), then extended to aVR, aVL, and aVF leads (Figure 1B), then I, II, and III leads to becoming total ECG bigeminy PVCs (Figure 1C). (Figure 1D), then into irregular PVCs (Figure 1E) lastly extended to runs of VT (Figure 1F). There is a mild renal impairment (serum creatinine: 2.86 and blood urea:95). The operator advised adding nitroglycerin IVI and diltiazem oral tablet. Despite there was a response but the recurrence was founded. The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 1: ECG tracings showing bigeminy PVCs with “Graded phenomenon right to left extension, upgrading” only started in V1-6 leads (A-tracing; green color), then in Leads: II, III, and aVF with V1-6 (B-tracing; blue color), then to all ECG leads (C-tracing; brown color).
Case no. 2: (Progressive Polymorphic Ventricular Tachycardia (Pvt))
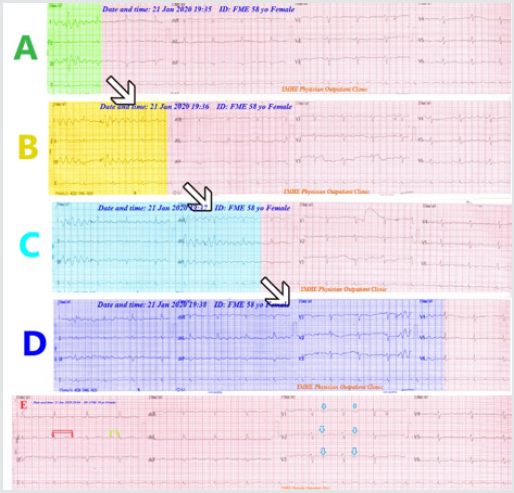
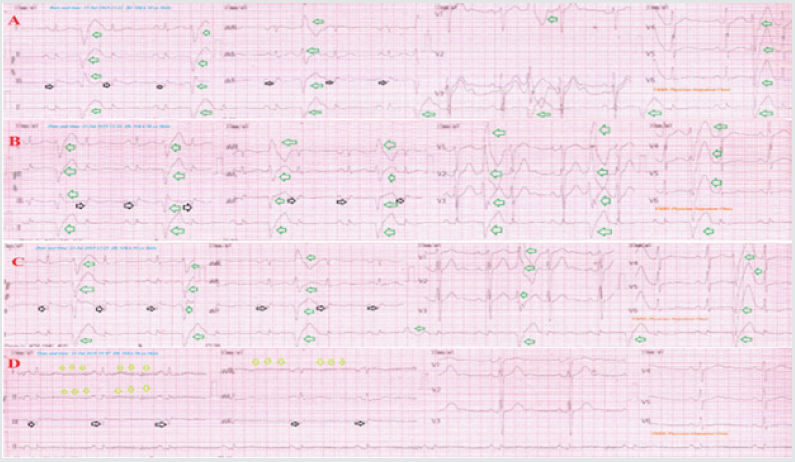
A 58-year-old married Egyptian housewife female patient presented to the POC with dizziness, dyspnea, and palpitations. The patient gave a history of psycho-familial troubles. Clinically, she had appeared myxedematos. There was sub-clinical hypothyroidism and congestive heart failure (CHF). Serial ECG tracings were taken which showed an interesting progressive polymorphic ventricular tachycardia (PVT) was described as: “Graded phenomenon left to the right extension, upgrading” (Figure 2). PVT initially started in part of I, II, and III leads (Figure 2A), then extended to the remaining part of I, II, and III leads (Figure 2B), then I, II, and III leads to then extended to part of aVR, aVL, and aVF leads (Figure 2C), lastly extend to V1,2, 3, and part of V4-6 (Figure 2D), then into irregular PVCs (Figure 2E) extended to runs of VT (Figure 2F). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 2: A-D ECG tracings; showing an interested progressive polymorphic ventricular tachycardia (PVT) “Graded phenomenon left to right extension, upgrading” started in part of I, II, and III leads (A-tracing; green color), then extended to the remaining part of I, II, and III leads (B- tracing; gold color), then extended to part of aVR, aVL, and aVF leads (C-tracing; light blue color), then extend to V1,2, 3, and part of V4-6 (D- tracing; dark blue color), E-tracing showing the disappearance of all PVT. There is evidence of QTc prolongation (470 ms, red rectangle and arrows) and prolonged R-interval (0.24 sec, lemon rectangle and arrows), superficial T-wave inversion in V1-3 leads.
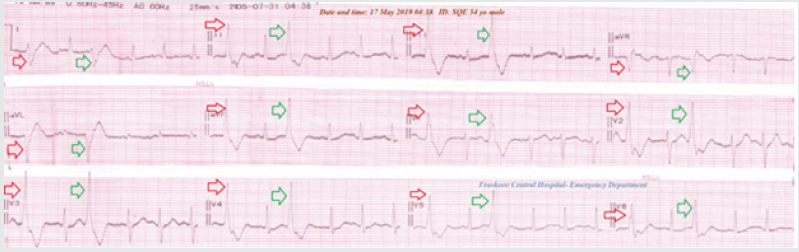
Case No. 3: (Progressive Bidirectional Sectors Of Tachycardia (BSOT))
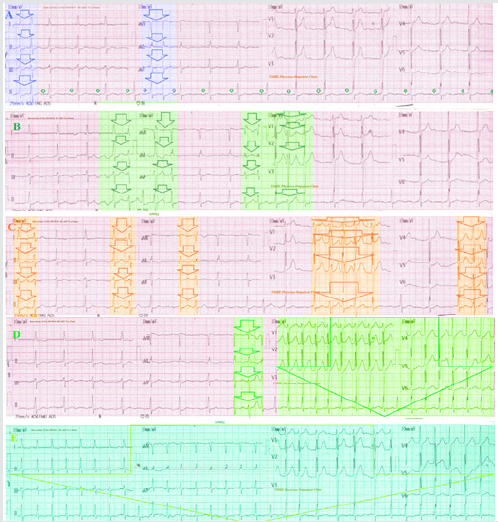
A 75-year-old married Egyptian housewife female patient presented to the POC with chest pain, dyspnea, and palpitations. The patient initially diagnosed as hypertensive crises with junctional tachycardia. Serial ECG tracings were taken which showed interesting progressive bidirectional sectors of tachycardia (PSOT) with a normal rhythm in between until becoming total tachycardia in all ECG tracing (Figure 3). PSOT initially started in first part of I, II, and III, aVR, aVL, and aVF leads (Figure 3A), then extended to last part of I, II, III, and aVR, aVL, and aVF and first part of, aVR, aVL, aVF, and V1-3 leads (Figure 3B), then first part of I, II, III, middle part of aVR, aVL, aVF and V1-3, and last part of I, II, III, and V4-6 leads (Figure 3C), then extend to last part of aVR, aVL, and aVF, and all V1-6 leads (Figure 3D), lastly it includes all ECG leads (Figure 3E). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 3: A-E ECG tracings showing “Graded phenomenon with an interested progressive bidirectional sectors of tachycardia (BSOT) with normal rhythm in between until become total tachycardia in the all ECG tracing” SOT initially started in first part of I, II, and III, aVR, aVL, and aVF leads (3 A tracing; blue color), then extended to last part of I, II, III, and aVR, aVL, and aVF and first part of, aVR, aVL, aVF, and V1-3 leads (3 B tracing; green color), then first part of I, II, III, middle part of aVR, aVL, aVF and V1-3, and last part of I, II, III, and V4-6 leads (3 C tracing; gold color), then extend to last part of aVR, aVL, and aVF, and all V1-6 leads (3 D tracing; green color), lastly it includes all ECG leads (3 E tracing; turquoise color).
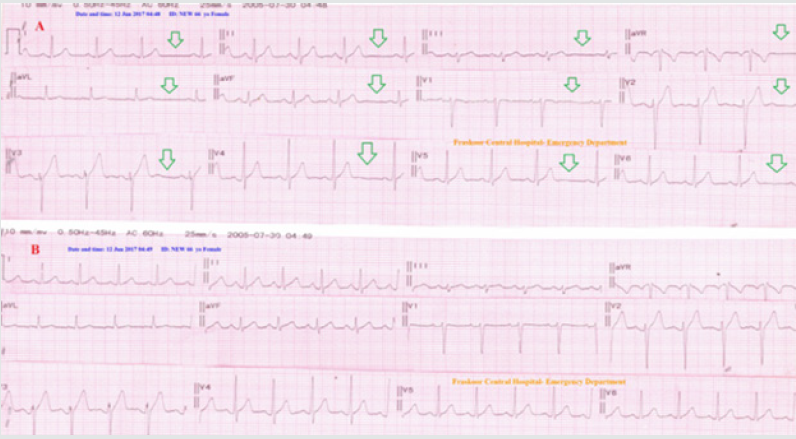
Case No. 4: (Intermittent Wandering Pacing Rhythm (Wpr) With Progressive Extension From Left To Right)
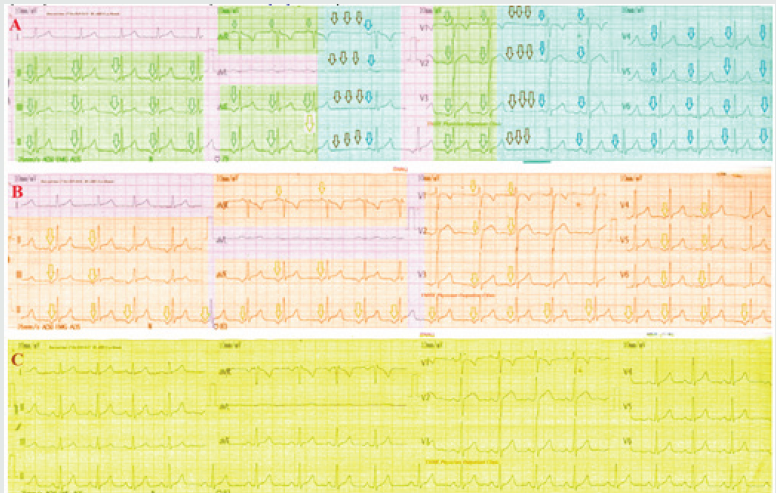
An 11-year-old Egyptian boy student patient presented to the POC with pleuritic chest pain. There was no history of heart disease. Serial ECG tracings were taken which showed an interesting intermittent Wandering pacing rhythm (WPR) with progressive extension from left to right. It progresses until becoming total junctional rhythm in all ECG tracing except lead I and aVL, then spontaneously normalized (Figure 4). WPR initially started in I, II, and first part of III, aVR, aVL, and aVF leads, then sinus bradycardia in the remaining part of aVR, aVL, and aVF leads, then junctional rhythm (JR) in part of V1-3, lastly sinus bradycardia in the remaining part of V-3, and all V4-6 leads (Figure 4A), then JR including all ECG tracing except lead I and aVL (Figure 4B), then spontaneously normalized (Figure 4C). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 4: A-C Serial ECG tracings were taken which showed an interesting intermittent Wandering pacing rhythm (WPR) with progressive extension from left to right. It progresses until becoming total junctional rhythm in all ECG tracing except lead I and aVL, then spontaneously normalized. WPR initially started in I, II, and first part of III, aVR, aVL,and aVF leads (green arrows and color), then sinus bradycardia in the remaining part of aVR, aVL, and aVF leads (black and blue arrows, and color), then junctional rhythm (JR) in part of V1-3 (green arrows and color), lastly sinus bradycardia in the remaining part of V-3, and all V4-6 leads (black and blue arrows, and color) (4 A. ECG tracing), then JR including all ECG tracing except lead I and aVL (4 B. ECG tracing), then spontaneously normalized (4 C. ECG tracing).
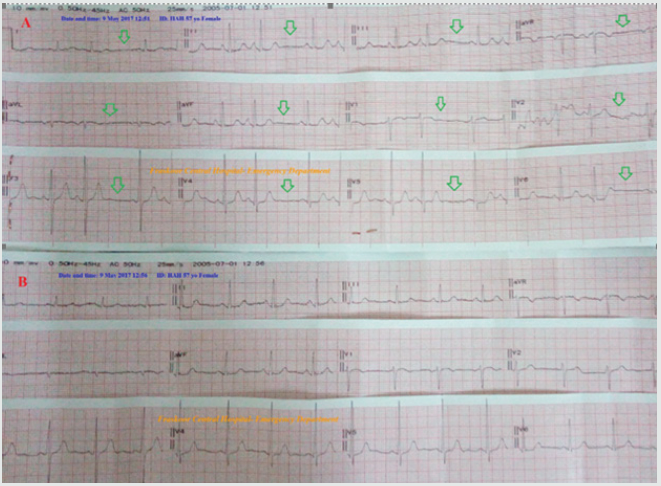
Case No. 5: (Progressive Accelerated Junctional Rhythm (Ajr) With The Right To The Left Extension)
A 37-year-old married Egyptian housewife female patient presented to the POC with irritable bowel syndrome with chest tightness, and palpitations. She gave a history of anxiety due to delayed infertility. The patient initially diagnosed as anxiety with a junctional rhythm. Serial ECG tracings were taken which showed progressive accelerated junctional rhythm (AJR) with the right to the left extension. with a normal rhythm in between until becoming total junctional rhythm in the all ECG tracing, then spontaneously normalized (Figure 5). JR initially started in V1-6 leads (Figure 5A), then extended to all ECG leads except aVL (Figure 5B), then spontaneously normalized in all ECG leads (Figure 5C). The patient advised for further electrophysiological study (EPS). For more details see Table 4, 5, and 6.
Figure 5: A-C Serial ECG tracings showed junctional rhythm (JR) with progressive extension from right to left. with a normal rhythm in between until becoming total junctional rhythm in all ECG tracing, then spontaneously normalized. JR initially started in V1-6 leads (green arrows and color), with the remaining are sinus rhythm (blue arrows and color) (5 A. ECG tracing), then extended to all ECG leads except (brown arrows and color) (5 B. ECG tracing), then spontaneously normalized in all ECG leads (5 C. ECG tracing; yellow color).
Case no. 6: (Fixed Trigeminy In Anxiety And Old Imi)
Figure 6: A-D ECG tracings; A-C tracings showing fixed trigeminy PVCs (green arrows) with evidence of inferior myocardial infarction (black arrows). D-tracing (within 30 hours after the first ECG) showing complete showing normalization of all above trigeminy PVCs. There is an ECG artifact (lemon arrows).
A 50-year-old married Egyptian male teacher patient presented to the POC with dizziness and palpitations. The patient appeared anxious. Recent history of psychological stress. There was a history of old MI. The ECG recordings were showing fixed trigeminy PVCs through all ECG leads with VR; 66 bpm (Figure 6A-C). ECG recordings were taken within 30 hours after the first ECG later and were the disappearance of trigeminy PVCs after oral nitroglycerin retard capsule (2.5 mg twice daily). (Figure 6D). No recurrence for above ECG trigeminy on later serial ECG tracings follows up. For more details see Table 4-6.
Case No 7 (Pvcs Type Up-Grading In Suspected Pulmonary Embolism In Thrombophilia)
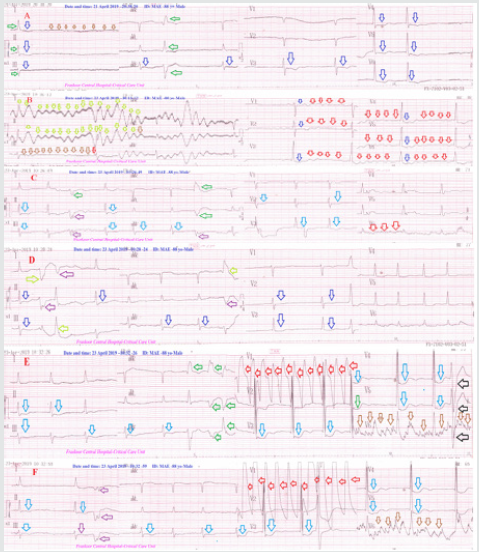
An 88-year-old married, worker, Egyptian male patient presented in the ER with tachypnea and palpitation. The patient gave a recent history of bilateral LL swelling. The patient has a history of hypertension, AF, multiple cerebrovascular strokes with bulbar palsy. At home, the patient missed his warfarin (3 mg). He was admitted to the ICU as suspected acute pulmonary embolism. Serial ECG tracings were done that showing PVCs type up-grading; A. tracing showing slow AF, sinus arrest, multiple PVCs, and inferior-anterior ST-segment depressions (Figure 7A). B. tracing showing polymorphic VT, AF waves, sinus arrest, and anterior ST-segment depressions (Figure 7B). C. tracing showing multifocal PVCs, inferior-anterior ST-segment depressions, and AF waves (Figure 7C). D. tracing showing inferior-anterior STsegment depressions and multifocal PVCs (Figure 7D). E. tracing showing runs of VT, inferior-anterior ST-segment depressions, and tremor artifact (Figure 7E). F. tracing showing runs of VT, inferior-anterior ST-segment depressions, multifocal PVCs, and tremor artifact (Figure 7F). Color duplex US showed extensive bilateral popliteal and leg veins. Plain Chest X-Ray view showed cardiomegaly, increased CTR, RV enlargement, RA enlargement bilateral enlargement of both pulmonary arteries, and oligemia of both lungs. Later echocardiography showed evidence of right-side dilatation with dysfunction. No more workup was done. The case was initially managed as APE. Unfortunately, the patient had died within 12 hours. For more details see Tables 4-6.
Figure 7: Serial ECG tracings showing PVCs type grading in suspected pulmonary embolism in thrombophilia; A. tracing showing slow AF, sinus arrest (brown arrows), multiple PVCs (green arrows), and inferior-anterior ST-segment depressions (blue arrows). B. tracing showing polymorphic VT (lemon arrows), AF waves (red arrows), sinus arrest (brown arrows), and anterior ST-segment depressions (blue arrows). C. tracing showing multifocal PVCs (green and purple arrows), inferioranterior ST-segment depressions (blue arrows), and AF waves (red arrows). D. tracing showing inferior-anterior ST-segment depressions (blue arrows) and multifocal PVCs (lemon and purple arrows). E. tracing showing runs of VT (red arrows), inferior-anterior ST-segment depressions (blue arrows), and tremor artifact (brown arrows). F. tracing showing runs of VT (red arrows), inferior-anterior ST-segment depressions (blue arrows), multifocal PVCs (purple arrows), and tremor artifact (brown arrows).
Case no. 8 (Fixed Pvcs Grading In Chf; Hexagimeny- Trigimeny- Trigimeny Hexagimeny: “6-3-3-6”)
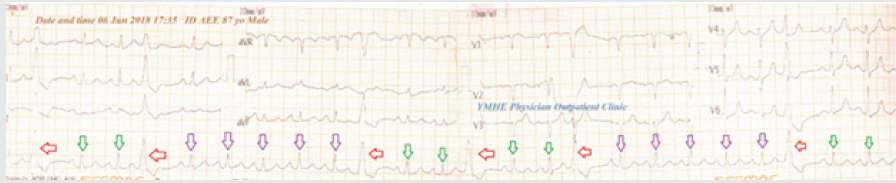
An 87-year-old married Egyptian male farmer presented to the POC with palpitations. There was a history of compensated CHF and cirrhotic liver disease. ECG tracing was taken which showed an interested fixed PVCs grading in CHF; starting as hexagimeny, then trigimeny, then trigimeny hexagimeny as: (6-3-3-6) in a serial fixed manner. (Figure 8). For more details see Tables 4-6.
Figure 8: ECG tracing was taken which showed an interested “fixed grading in PVCs (red arrows); starting as hexagimeny, then trigimeny, then trigimeny (green arrows) hexagimeny (purple arrows) as: (6-3-3-6) in a serial fixed manner.
Case No. 9: (Fixed Pvcs Grading In Chf; Quadrigimeny- Bigimeny- Bigimeny Quadrigeminy “4-2-2-4”)
A 75-year-old married Egyptian female housewife presented to the POC with dizziness. There was a history of compensated chronic heart failure (CHF) and obstructive sleep apnea (OSA). ECG tracing was taken which showed an interesting fixed grading in PVCs; starting as Quadrigimeny-bigimeny-bigimeny quadrigimeny as: (4-2-2-4) in a serial fixed manner. (Figure 9). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 9: ECG tracing was taken which showed an interested “fixed grading PVCs (red arrows); starting as Quadrigimeny (purple arrows)-bigimeny-bigimeny (green arrows) quadrigimeny (purple arrows)” as: (4-2-2-4) in a serial fixed manner.
Case No. 10: (Non-fixed PVCs variation in grading in angina post-tramadol)
A 70-year-old married Egyptian male carpenter presented to ER with chest pain, dyspnea, and dizziness. He gave a recent history of ingested 3 tablets of oral tramadol (100 mg). There was a history of urinary bladder carcinoma. ECG tracing was taken which showed an interested “Non-fixed PVCs variation in grading” (Figure 10). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Case No. 11: (Fixed bigeminal-quadrigeminal PVCs grading)
A 54-year-old married Egyptian male governmental officer presented to ER with palpitations. He gave a history of CHF. ECG tracing was taken which showed an interested “Fixed bigeminalquadrigeminal PVCs grading” (Figure 11). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 11: ECG tracing was taken which showed an interested “fixed bigeminal-quadrigeminal PVCs grading”.
Case No. 12: (Up-grading PVCs in CHF)
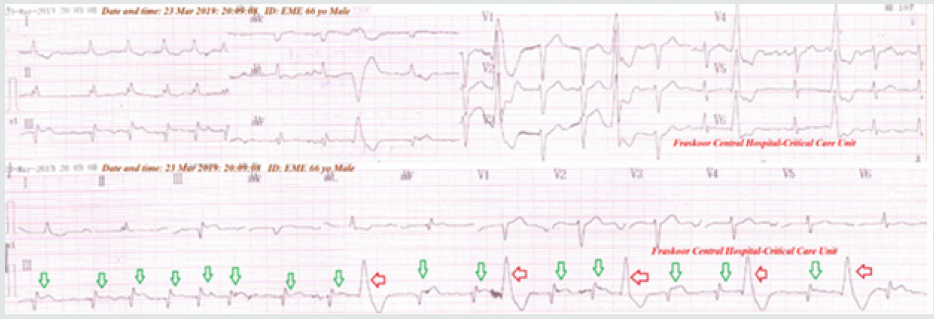
A 66-year-old married Egyptian male carpenter presented to the orthopnea. The patient had a recent history of CHF. He was admitted to the ICU as a CHF. Serial ECG tracing was taken which showed Up-grading from less frequent (trigeminy) to more frequent PVCs (bigeminy). The patient advised for further electrophysiological study (EPS) (Figure 12). For more details see Tables 4-6.
Figure 12: ECG tracing was taken which showed Up-grading PVCs from less frequent (trigeminy) to more frequent PVCs (bigeminy).
Case No. 13: (Insignificant isolated PVCs)
A 43-year-old married Egyptian female housewife presented to the POC with palpitations. There was a history of psycho-familial troubles. ECG tracing was taken which showed insignificant isolated PVCs. (Figure 13). The patient was managed with reassurance. For more details see Tables 4-6.
Case No. 14: (Insignificant isolated PVCs but important)
A 60-year-old married Egyptian female housewife presented to the ER with dizziness. There was a history of compensated chronic renal failure (CRF) on regular hemodialysis. She was admitted to ICU as symptomatic bradycardia. ECG tracing was taken which showed sinus bradycardia with few PVCs (Insignificant isolated PVCs but important) (Figure 14A). The above abnormalities reversed after atropine iv injection (1 mg). (Figure 14B). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 14: ECG tracings were taken which showed sinus bradycardia with few PVCs (an insignificant isolated PVCs but important) (tracing 14A). The above abnormalities reversed after atropine iv injection (1 mg). (tracing 14B).
Case No. 15: (Down-grading with less frequency of PVCs in CHF)
A 66-year-old married Egyptian male electrician presented to the orthopnea. The patient had a recent history of CHF. He was admitted to the ICU as a CHF. Serial ECG tracings were taken which showed Down-grading with less frequency of PVCs with ECG strip (Figure 15). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 15: ECG tracings were taken which showed ”down-grading PVCs” with ECG strip (red arrows). There is wavy triple an electrocardiographic sign (Yasser sign) for hypocalcemia in the anterior leads esp. V4-6 (green arrows).
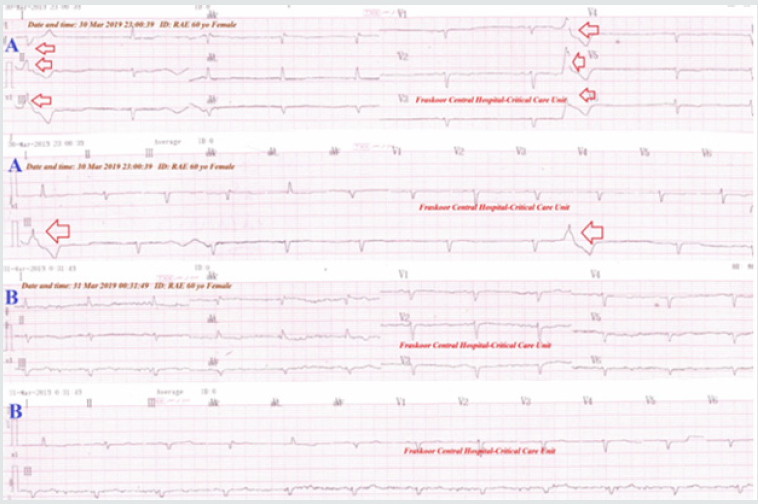
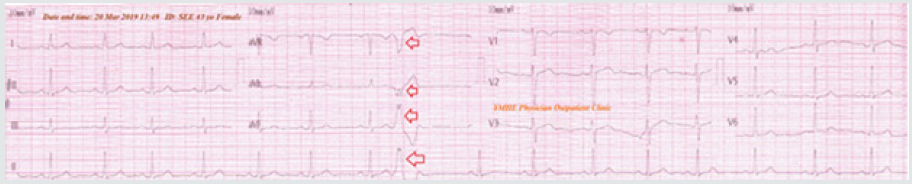
Case No. 16: (Sinus arrhythmia spontaneously graded to normal)
A 66-year-old married housewife Egyptian female patient presented to the ER for follow up. The ECG recordings were showing sinus arrhythmia (Figure 16A). ECG recordings were taken one minute later and were completely normal without any medications (Passing phenomenon) (Figure 16B). The patient was only managed with reassurance. No recurrence for above ECG abnormalities on later serial ECG tracings follows up. For more details see Tables 4-6.
Figure 16: A. the initial ECG tracing showing sinus arrhythmia (green arrows) and with VR; 92 bpm. B. ECG tracing one minute later showing spontaneously normalization of all above changes.
Case No 17: (Sinus arrhythmia spontaneously graded to normal)
A 57-year-old married housewife Egyptian female patient presented to the ER for inguinal hernia preoperative preparation. The ECG recordings were showing sinus arrhythmia (Figure 17A). ECG recordings were taken one minute later and were completely normal without any medications (Passing phenomenon) (Figure 17B). The patient was only managed with reassurance. No recurrence for above ECG abnormalities on later serial ECG tracings follows up. For more details see Tables 4-6.
Figure 17: A. the initial ECG tracing showing sinus arrhythmia (green arrows) with VR; 76 bpm. B. ECG tracing one minute later showing spontaneously normalization of all above changes.
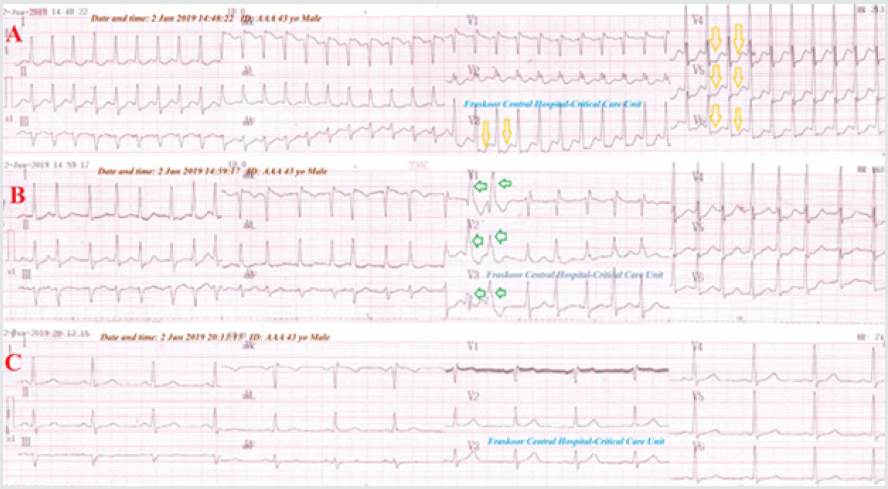
Case No 18: (PSVT spontaneously graded to AF)
A 43-year-old married Egyptian male worker presented to ER with palpitations and headache. He was a heavy cigarette smoker. He was admitted to the ICU as PSVT with HC. ECG tracing was taken which showed an interesting “PSVT spontaneously graded to AF” with ST-segment depressions in V3-6 leads (Figure 18). The patient advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Figure 18: ECG tracings showing PSVT with ST-segment depressions in V3-6 leads (A. tracing; gold arrows) spontaneously graded to AF with few PVCs couplets (B. ECG tracing; green arrows), with complete normalization of all above changes with conversion to NSR after treatment (C. tracing).
Case No 19: (JT spontaneously graded to sinus tachycardia)
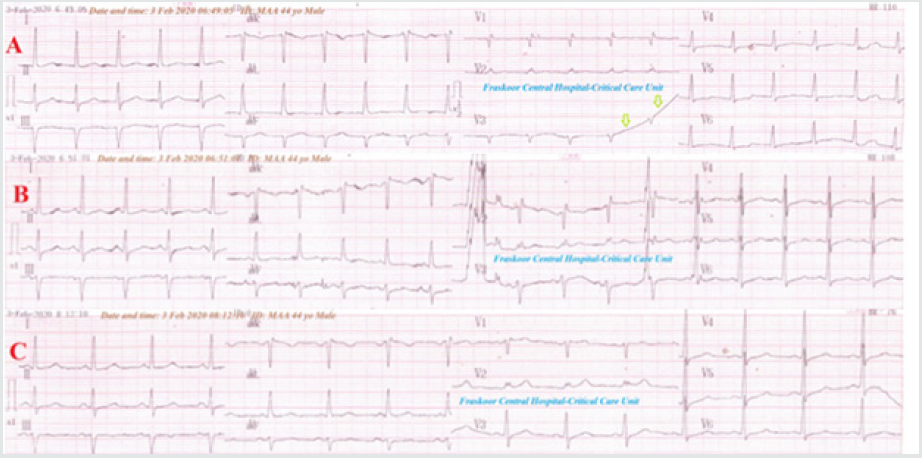
A 44-year-old married, driver, heavy cigarette smoker, Egyptian male patient presented in the ER with acute severe chest pain and palpitation. The chest pain was anginal The patient gave a recent history of using substance abuse. He was admitted to the ICU and managed in the ICU as unstable angina. ECG tracing was taken which showed an interested “JT spontaneously graded to sinus tachycardia” (Figure 19). For more details see Tables 4-6.
Figure 19: ECG tracings showing JT (A. tracing) spontaneously graded to sinus tachycardia (B. ECG tracing), with complete normalization of all the above changes with conversion to NSR after treatment (C. tracing).
Case No. 20: (Progressive AJR with the left to right extension in pleurisy and cold)
A 17-year-old single Egyptian male student presented to the POC with pleuritic chest pain. The patient had a recent history of a common cold. Serial ECG tracings were taken which showed progressive AJR with the left to the right extension. with a normal rhythm in between until becoming total JR in the all ECG tracing, then spontaneously normalized (Passing phenomenon). JR initially started in I, II, III, aVF, and part of V3-6 leads, except aVR, aVL, V1-2, and the remaining part of V3-6 lead, then extended to all ECG leads, then spontaneously normalized in all ECG leads. No recurrence for above ECG abnormalities on later serial ECG on follow up. The patient advised for further electrophysiological study (EPS. For more details see Tables 4-6.
Case No 21. (AJR and sinus arrhythmia with progressive extension from left to right in the prolapsed cervical disc)
A 56-year-old married Egyptian male teacher patient presented to POC with musculoskeletal chest pain. Chest pain associated with bilateral arm pain with weakness, paraesthesia, and numbness. The patient gives a history of lumbosacral herniated disc prolapse with the surgical repair 9 years ago. Local tenderness was elicited. The ECG recordings were showing AJR in the inferior leads; II, III, aVF (inverted P-wave), and aVR (upright P-wave) with sinus arrhythmia. ECG recordings were taken two minutes later and were completely normal without any medications (Passing phenomenon). MRI of the cervical spine showing herniated disc prolapse between C4 and C5 vertebrae with spinal stenosis. No recurrence of accelerated junctional rhythm on later serial ECG tracings. The patient was referred to the neurosurgeon after reassurance for further evaluation, management, and advised for further electrophysiological study (EPS). For more details see Tables 4-6.
Case No 22. (AJR with progressive extension from left to right in myositis)
A 43-year-old married housewife Egyptian female patient presented to POC with musculoskeletal chest pain. Local tenderness was elicited. The ECG recordings were showing AJR in the inferior leads ( II, III, aVF) and all anterior leads (V1-6). ECG recordings were taken two minutes later and were completely normal without any medications (Passing phenomenon). There are leukocytosis (14400) and increased CPK (473 IU/L). The patient was managed only with diclofenac potassium (tab., 25 mg/8 hours for 5 days). No recurrence for above ECG abnormalities on later serial ECG on follow up. For more details see Tables 4-6.
Case No 23: (AJR with progressive extension from left to right in pleurisy and cold)
A 47-year-old married male heavy smoker farmer Egyptian patient presented to the POC with pleuritic chest pain. The patient had a recent history of a common cold. Chest examining was showing pleuritic rub on listening. The ECG recordings were showing AJR with progressive extension from left to right (P-wave inversion through all ECG leads except aVR and V1-2 (upright P-wave) with VR;70 bpm. ECG recordings were taken one minute later and were completely normal without any medications (Passing phenomenon). Pleurisy was managed only with diclofenac (tab., 25 mg/8 hours for 5 days). No recurrence for above ECG abnormalities on later serial ECG tracings follows up. For more details see Tables 4-6.
Case No 24: (Down-Graded bigeminal RBBB)
A 70-year-old, heavy cigarette smoker, Egyptian farmer, the male patient presented in the ER with dizziness. The patient gave a history of IHD and HTN. The patient admitted to the intensive care unit (ICU). The initial emergency and serial ECG tracing showed down-graded bigeminal RBBB with ST-segment depression in III and V4-6 leads. He managed with nitroglycerin IVI. The next ECG tracing showed RBBB with trigeminy but with normalization of ST-segment depression. The third ECG tracing was taken after 30 minutes of nitroglycerin IVI within 6 hours of the ICU. It showed nearly complete disappearance of the above Abnormalities. The echocardiographic report showed evidence of IHD with apical and lateral wall hypokinesia with diastolic dysfunction and low ejection fraction (52%). The patient continued on nitroglycerin retard (2.5 capsules; BID) on discharge with no future problems. For more details see Tables 4-6.
Case No 25: (Up-grading PVCs in acute pulmonary embolism)
An 80-year-old, Egyptian worker, the male patient presented in the ER with tachypnea and acute confusion. His wife gave a recent history of diazepam amp (10 mg) injection for irritability. The patient admitted to the ICU with suspected acute pulmonary embolism. The initial emergency and serial ECG tracing showed RBBB with PVCs up-grading from less frequent to more frequent PVCs (bigeminy) with ST-segment depression in V4-6 leads. He managed as an acute pulmonary embolism. No recurrence for PVCs on later serial ECG tracings follows up. For more details see Tables 4-6.
Case No 26: (Down-grading PVCs in CHF and CVA)
An 82-year-old married housewife Egyptian female patient presented to the ER with orthopnea and hemiplegia. The patient gave a history of CHF and IHD. The patient admitted to the ICU as CVA with CHF. The initial emergency and serial ECG tracing showed Down-grading PVCs from more frequent (bigeminy) to less frequent PVCs (pentageminy) with wavy triple an electrocardiographic sign (Yasser sign) for hypocalcemia in the all leads. The echocardiographic report showed evidence of IHD with global hypokinesia, systolic dysfunction, and low ejection fraction (45%). For more details see Tables 4-6.
Case No 27: (Non-fixed variation on grading in CHF)
A 60-year-old married housewife Egyptian female patient presented to the POC with dizziness and palpitations. The patient gave a history of CHF, IHD, and HTN. The patient admitted to the ICU as frequent symptomatic PVCs. The initial emergency and serial ECG tracing showed Non-fixed variation on grading in CHF The echocardiographic report showed evidence of IHD with mild hypokinesia with ejection fraction (58%). For more details see Tables 4-6..
Case No 28: (Non-significant PVCs in old MI)
A 64-year-old, heavy smoker, Egyptian carpenter, the male patient presented in the ER with chest pain and palpitations. The patient admitted to the ICU as unstable angina. The initial emergency and serial ECG tracing showed Non-significant PVCs in evidence of old MI (pathological Q-wave in inferior leads; II, III, and aVF) leads. He managed as unstable angina. No recurrence for PVCs on later serial ECG tracings follows up. For more details see Tables 4-6..
Case No1 29 (Sinus arrhythmia spontaneously graded to normal)
A 34-year-old married worker Egyptian male patient presented to the ER for blood pressure follow up. The ECG recordings were showing sinus arrhythmia. ECG recordings were taken four minutes later and were completely normal without any medications (Pass phenomenon). The patient was only managed with reassurance. No recurrence for above ECG abnormalities on later serial ECG tracings follows up. For more details see Tables 4-6..
Case No 30 (Sinus arrhythmia spontaneously graded to normal with anxiety)
An 85-year-old married housewife Egyptian female patient presented to the emergency room with palpitation. The patient had a recent history of anxiety. ECG recordings were showing sinus arrhythmia. ECG recordings were taken three minutes later and were completely normal without any medications (Pass phenomenon). The patient was only managed with reassurance. No recurrence for above ECG abnormalities on later serial ECG tracings follows up. For more details see Tables 4-6.
Results, Findings, and Discussion
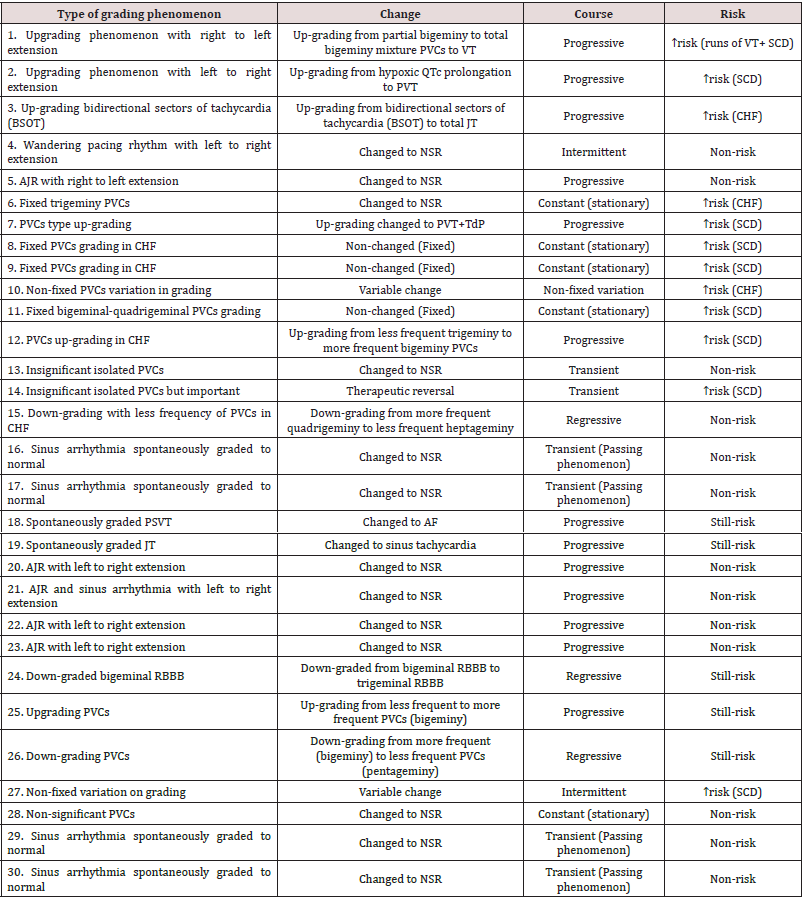
1. The Changes In “Graded Phenomenon” Is Classified Into:
1. Up-grading; 20% (6 cases), 2. Down Graded; 10% (3 cases),
3. Changed to NSR; 43.33% (13 cases), 4. Changed to AF; 3.33% (1 case), 5. Changed to sinus tachycardia; 3.33% (1 case), 6.
Therapeutic reversal; 3.33% (1 case), 7. Fixed change; 10% (3
cases), 8. Variable change; 6.67% (2 cases) (Figure 20).
2. The Course in “Graded Phenomenon” is Classified into: 1. Progressive; 43.33% (13 cases), 2. Regressive; 10% (3 cases), 3. Intermittent; 6.67% (2 cases), 4. Constant; 16.67% (5 cases), 5. Transient; 20% (6 cases), Non-fixed variation; 3.33% (1 cases) (Figure 21),
Figure 21: showing the graphical presentation for the course progression in the “Graded phenomenon”.
3. The risk in “Graded phenomenon” is classified into: 1.
High risk; 40% (12 cases), 2. Non-risk; 43.33% (13 cases), 3.
Still-risk; 16.67% (5 cases) (Figure 22).
4. Age averages mean (58.3), median (60), and, mode (60).
5. Sex averages: male Sex predominance: 17 cases (56.67%).
6. The Age mean:58.3 years with male Sex predominance;17
cases (56.67%).
7. The changes in “Graded phenomenon” are classified into:
Up-grading; 20%, down-graded; 10%, changed to NSR; 43.33%,
changed to AF; 3.33%, changed to sinus tachycardia; 3.33%,
therapeutic reversal; 3.33%, fixed –change; 10%, and variable
change; 6.67%.
8. The risk in the “Graded phenomenon” is either high
(40%), non-risk (43.33%), or still-risk (16.67%).
9. The course in the graded phenomenon is either
progressive (43.33%), regressive; 10%, intermittent; 6.67%,
constant; 16.67%, transient; 20%, and non-fixed variation;
3.33%.
10. The following are the principals for understanding the
“Graded phenomenon”:
a. The “Graded phenomenon” (Yasser’s phenomenon)
is a novel electrocardiographic phenomenon change the
arrhythmia directory.
b. It is a crucial step for understanding the arrhythmia.
c. The phenomenon is a new strong guide for monitoring
and follows up arrhythmic patients.
d. The principal of “Graded phenomenon” is based on
catching the graded changes in serial ECG tracings or even
single one regarding the arrhythmias.
e. The “Graded phenomenon” is a crucial step to repeat and
reassessment arrhythmia management.
f. The graded changes in the serial ECG tracings or even
single one regarding arrhythmias constitute the main topic
for this research.
11. The changes in “Graded phenomenon” are:
a. Up-grading: It is meaning that the change either from
low serious arrhythmia to higher serious arrhythmia, or more
extension for the current serious arrhythmia, or ending to
serious arrhythmia or just extension for a benign arrhythmia
e.g. case No. 1. Up-grading may be included an up-grading type
of arrhythmia as in case No. 7.
b. Down-grading: It is meaning that the change either from
higher serious arrhythmia to low serious arrhythmia, or less
extension for the current serious arrhythmia, or ending to the
benign or non-serious arrhythmia e.g. case No. 15.
c. Fixed change: It is meaning that the current arrhythmia is
constant in the serial ECG or even the single ECG tracing e.g.
case No. 6.
d. Spontaneously changed to normal sinus rhythm: It
is meaning that the current arrhythmia is spontaneously
changed to normal sinus rhythm with no uses of medications
or therapeutic maneuvers like DCC and Valsalva’s e.g. case No.
16 and17.
e. Spontaneously changed to another arrhythmia e.g. sinus
tachycardia e.g. case No. 19 and atrial fibrillation e.g. case No.
18.
f. Therapeutic reversal: It is meaning that there is a new
arrhythmic change after using the traditional antiarrhythmic
e.g. case No. 14.
g. The extension for arrhythmia in “Graded phenomenon”
are : The up-grading phenomenon with the right to left
extension: It is meaning that the arrhythmic change starting
from the right side of ECG tracing directed toward its left side
e.g. case No. 1.
h. The up-grading phenomenon with the left to right
extension: It is meaning that the arrhythmic change starting
from the left side of ECG tracing directed toward its right side
e.g. case No. 2.
i. Up-grading bidirectional sectors of tachycardia (BSOT): It
is meaning that the arrhythmic change starting as sectors of
tachycardia then gradually extend to both left and right side
of ECG tracing until becoming complete tachycardia e.g. case
No. 3.
j. Intermittent Wandering pacing rhythm with the left
to right extension: It is meaning that the change occurring
intermittent manner then extends from left to right e.g. case
No. 4.
12. The risk in arrhythmia with “Graded phenomenon” are:
a. High: This is meaning that there will be possible serious
outcomes like; sudden cardiac deaths congestive heart failure,
Torsades de pointes, and VT ventricular tachycardia e.g. case
No. 1, 2, and 7.
b. Non-risk: This is meaning that there will not be possible
serious outcomes e.g. case No. 1, 2, and 7.
c. Still-risk: This is meaning that there are no current
possible serious outcomes but maybe with passing the time
e.g. case No. 18, 24, and 26.
Conclusion and Recommendation
Graded phenomenon (Yasser’s phenomenon) is a novel electrocardiographic phenomenon change the arrhythmia directory. It is a crucial step for understanding arrhythmia. The phenomenon is a new strong guide for monitoring and follows up arrhythmic patients in cardiovascular patients. There are interlacing correlations between the “passing phenomenon” [49] and the current “Graded phenomenon” especially in cases of arrhythmia that is spontaneously changed to normal sinus rhythm with no uses of medications or therapeutic maneuvers like DCC and Valsalva’s e.g. case No. 16 and17. Electrophysiology studies (EPS) is recommended for more future study and understanding the “Graded phenomenon”. Physiological study for the cellular electrolytes may be advised future options for the “Graded phenomenon”.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
I wish to thank Dr. Ameer Mekkawy; M.sc. for technical support, and both the emergency department and critical care unit nurses who make extra-ECG copies for helping me.
Read More About Lupine Publishers Journal of Anesthesia Please Click on Below Link:
https://lupine-publishers-anesthesia-pain.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.