Lupine Publishers| Journal of Gastroenterology and Hepatology
Short Communication
Obesity represents a dangerous public health concern all over the universe. The World Health Organization suggests that, by 2015, approximately 2.3 billion adults will be overweight and more than 700 million will be obese [1]. Prevalence of obesity continues to rise and obesity has become the second leading cause of death in the West [2]. Obesity is associated with numerous comorbidities affecting virtually every organ system, including hypertension, type II diabetes mellitus, coronary artery disease, dyslipidemia, certain cancers, and ultimately increased mortality [3]. Obese women of reproductive age are a specific group at risk for a host of obesityrelated reproductive and obstetric complications, such as infertility, early miscarriage, gestational hypertension and diabetes mellitus, pre-eclampsia, preterm birth, and intrauterine fetal demise [4].
Bariatric surgery has been recently proven to decrease mortality in postoperative patients when compared to obese controls and is, thus, a promising weapon in the fight against obesity [5]. Over 80 %of bariatric surgical patients are women with obesity in their reproductive years [6]. Obesity adversely affects fertility; the rapid weight loss following bariatric surgery can increase fecundity. To combat reproductive complications of obesity, the American College of Obstetrics and Gynecology advocates weight loss prior to conception and acknowledges bariatric surgery as preliminarily promising in prepregnancy obesity treatment [7]. Bariatric surgery has become a cornerstone in the management of morbid obesity and is safely recommended for obese women of childbearing age [8].
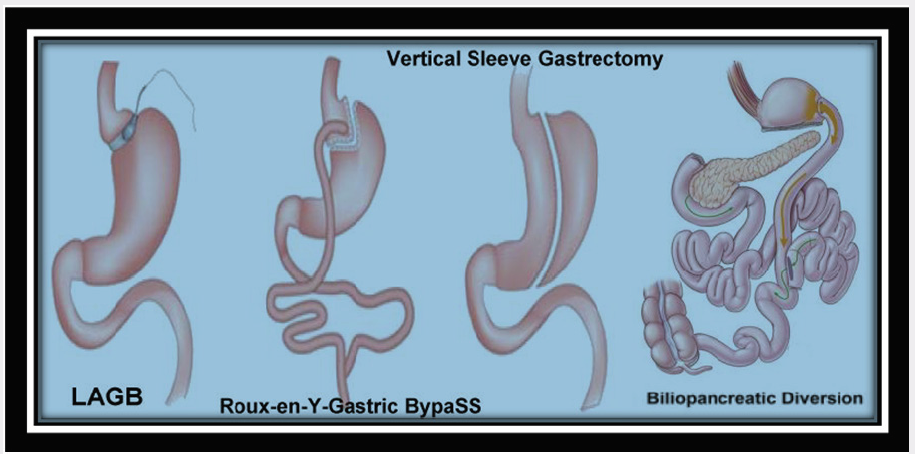
Procedures for bariatric surgery are traditionally categorized into three groups (Figure 1). The aim of the first group of procedures is to restrict energy intake by reducing gastric capacity. This includes the laparoscopic adjustable gastric band (LAGB). The Roux-en-Y gastric bypass (RYGB) is another type, which combines food restriction with a certain degree of malabsorption by shortening the length of the intestinal tract. The third group includes vertical sleeve gastrectomy (VSG). The Laparoscopic Sleeve Gastrectomy is performed by removing approximately 80 percent of the stomach. The remaining stomach is a tubular pouch that resembles a banana and the fourth type is biliopancreatic diversion. The most performed procedures today are the LAGB and the RYGB [9].
Restrictive approaches like vertical banded gastroplasty and laparoscopic adjustable gastric banding are designed to restrict caloric intake, whereas primarily malabsorptive procedures such as Biliopancreatic diversion with or without duodenal switch promote weight loss by decreasing nutrient absorption [10]. Reports of pregnancy after bariatric surgery demonstrated concerning complications related to poor maternal nutritional status, including anemia, neural tube defects, and intrauterine growth retardation [11]. In addition, a case of gastrointestinal bleeding after vertical banded gastroplasty and reports of fatal bowel obstruction secondary to internal intestinal herniation after Roux-en-Y gastric bypass caused further alarm among both bariatric surgeons and obstetricians alike [12].
Reproductive Management after Bariatric Surgery
a) Operation-to-birth intervals of less than 2 years were associated with higher risks for prematurity [13] because women after bariatric surgery suffer from nutritional deficiencies may be rather grave and may involve the developing foetus [14].
b) Reliable contraception after the operation. During this period there is a need for the use of reliable contraception. As there is a risk for malabsorption of hormones taken orally, the combined and progestogen-only pills are contraindicated, and displaced by non-oral hormonal contraception or non-hormonal methods, including intrauterine devices and condoms [15].
c) Nutritional monitoring and supplementation tailored to the type of bariatric operation performed with a specific focus on keying out and treating deficiencies in iron, folic acid, B12, calcium, and vitamin D both pre- and post-conception.
d) Recommendations during pregnancy: one standard prenatal vitamin daily, which may include or should be supplemented with the following 400 μg folate daily for all reproductive-aged women 50-100 mg elemental iron daily for menstruating and pregnant women 1,000 mg calcium daily for all postoperative patients, 60 g of dietary protein daily for pregnant patients.
e) Low threshold for suspicion of intestinal obstruction during pregnancy. Image via CT scan and surgical exploration as needed.
f) Close follow up of weight changes during gestation and postpartum cooperation with high-risk obstetrical colleagues in patient management.
Read More About Lupine Publishers Journal of Gastroenterology and Hepatology Please Click on Below Link: https://currenttrendsingastroenterology.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.