Lupine Publishers| Journal of Gastroenterology and Hepatology
Abstract
Aim : To determine the aetiologies of acute upper gastrointestinal bleeding (UGIB) in a setting highly endemic for hepatitis B and to describe actual clinical practices in a resource-limited setting.
Patients and methods: This study was conducted in two parts. The first part was retrospective from January 1st 2010, to December 31st 2019 on the epidemiological profile of UGIB and the second was a prospective study from December 1st 2017 to May 31st 2018 to evaluate, in a blinded experiment, the actual clinical practices in front of an acute UGIB at the emergency units in Yaounde (Cameroon), and included: recognizing UGIB, assessing for severity, taking emergency measures and prescribing emergency Eosogastroduodenal endoscopy (EGDE).
Results : During the retrospective period, 506 patients (prevalence of acute UGIB in the services 5.6%) were included of which 71.3% were men (sex ratio 2.5). The mean age was 49.9 +/- 8 years. Haematemesis was inaugural in 350 patients (69.1%), nonsteroidal anti-inflammatory drugs were the main risk factor in 297 (43.6%), in 78 (15.4%), this was a second episode. Clinical parameters showed initial instability in 435 patients (85.9%) and haemoglobin (Hb) was <7g/dl in 359 (83.4%). EGDE was performed in 203 patients (40.2%), the main causes of UGIB were lesions of portal hypertension in 111 (44.7%), followed by peptic ulcers in 108 (43.5%). Treatment was mainly medical. However, 94 patients (84.7%) with portal hypertension lesions received endoscopic treatment, mainly by injection of sclerosing agent (69.1%), as well as 13 (1.2%) with peptic ulcers, mainly by isolated injection of dilute adrenaline (1: 10,000) in 11 (84.6%). A total of 75 patients (14.8%) died. The second part concerned 74 patients admitted for acute UGIB at the emergency services of five hospitals in Yaounde. To recognize UGIB, a digital rectal examination was done in 43 patients (58.1%), no patient received a nasogastric tube. For assessment of severity, blood pressure was taken in 73 patients (98.6%), pulse rate in 61 (82.4%), respiratory rate in 17 (23%), saturation in 17 (23%), no patient had prognostic scores in their record. For resuscitation measures, 10 patients (13.5%) received a double peripheral venous line, 20 (27%) were filled with crystalloids, restrictive blood transfusion (Hb < 7 g /dl) was carried out in 24 out of 27 patients (88.9%), 9 (12.2%) received nasal oxygen therapy. EGDE was carried out in 43 patients (60.6%), all beyond 24 hours and none had a prognostic score (Forrest or Rockall).
Conclusion: Rupture of oesogastric varices plays a significant role in the occurrence of UGIB in areas with high hepatitis B endemicity, with exceptional severity and high mortality among young people. The lack of qualified human resources and insufficient technical facilities constitute a serious problem. Locally applicable protocols are needed. In the long term, eliminating viral hepatitis B and C should reduce the prevalence of UGIB
Keywords:Gastrointestinal Bleeding; Hepatitis B Virus; Portal Hypertension; Limited Resources; Endoscopy; Clinical Practice.
Background
Acute gastrointestinal bleeding is one of the major medical and surgical emergencies whose severity should never be underestimated [1]. In approximately 80% of cases, acute gastrointestinal bleeding is of high origin, i.e. the aetiology of the bleeding is located upstream of the duodenojejunal angle or Treitz angle [2]. Acute upper gastrointestinal bleeding (UGIB) is the most frequent emergency in hepato-gastroenterology and remains a major cause of mortality, despite improvements in technical facilities, the mortality rate remains stable at about 10-15% [1-4]. The UGIB is exteriorized in 66% of cases in the form of hematemesis and the aetiologies involved are varied [2,5-7]. In the West, the proportion of peptic ulcers is significantly high. Indeed, the most common causes of acute UGIB are non-varicose (80-90%) and include gastric and duodenal ulcers in 20-50% [2,3,5-7]. Contrarily, in sub-Saharan Africa, the proportion of portal hypertension lesions is significant [8,9]. The impact of chronic hepatitis B virus (HBV) infection in this highly endemic area is significant. In highly endemic countries, ≥8% HBsAg positivity, the HBV-related disease burden is due to liver cancer and cirrhosis in adulthood, responsible for portal hypertension. The majority (80%) of the world population lives in high- or intermediate-endemic areas [10]. The way to handle acute UGIB is well codified. Gastrointestinal bleeding must be recognised, its severity assessed, and blood loss compensated. Finally, the cause of the bleeding must be found and treated [1,2,7,11]. The diagnostic approach, non-specific measures to prevent or treat haemorrhagic shock and specific haemostasis measures according to the aetiology of UGIB are often not all implemented in resources limited countries and this has an impact on evolution and prognosis. Based on data collected in the files of patients admitted in emergency and those obtained following the daily clinical practice of emergency staff, the study aimed to highlight the epidemiology and actual management of acute UGIB in our context dominated by HBV infection and limited resources.
Methods
A retrospective collection of data contained in the files of patients admitted for acute UGIB at the Yaounde Central Hospital (Cameroon) between January 1st2010 and December 31st2019, was carried out. Located at the heart of the city of Yaounde, the Yaounde Central Hospital (YCH) was created in 1930. It is the largest public referral hospital in Cameroon with capacity of …. Beds that also acts as a teaching hospital. It houses several services including the Hepato-gastroenterology service with a capacity of 34 beds, three university specialists, four general practitioners and several permanent workers and residents. This service has an upper and lower gastrointestinal endoscopy room and endoscopy equipment. The variables recorded included: demographics (age, sex); clinical and biological characteristics (onset of UGIB, history of bleeding, physical parameters of bleeding severity, and haemoglobin levels on admission); Esogastroduodenal endoscopy (EGDE) findings; specific management of the cause of the bleeding and outcomes (Table1).
Table 1: Clinical and biological parameters of 506 patients admitted at the Yaounde Central hospital for a recognized acute UGIB.
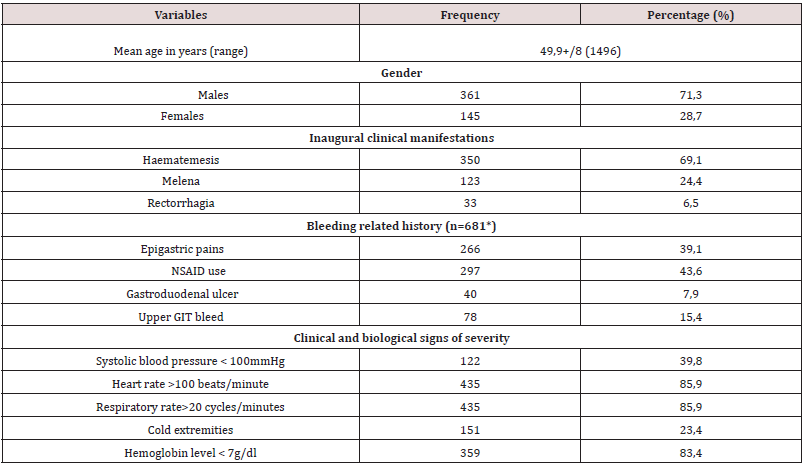
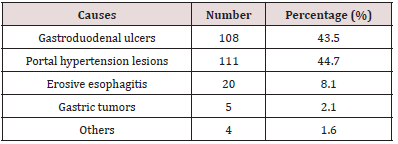
Table 2: Main causes of acute UGIB at the Yaounde Central Hospital amongst 203 patients who had an EGD.
The second component, cross-sectional and observational blinded experiments, conducted from December 1st 2017 to May 31st 2018, assessed the diagnostic approach and actual management of patients admitted for acute UGIB in five hospitals of different categories (1st to 3rd) of the Cameroonian health pyramid, in the city of Yaounde. Twenty (20) doctors and 39 nurses in the emergency service who managed 74 patients admitted for acute UGIB were followed. The elements to take care of acute UGIB included recognition of acute UGIB by placing a nasogastric tube or performing a digital rectal exam; assessment of severity by clinical criteria (taking blood pressure (BP), pulse rate (PR), respiratory rate (RR) and room oxygen saturation (SPO2), Glasgow- Blatchford score; fluid resuscitation and transfusions (double venous line, crystalloids filling, proton pump inhibitors (PPI) or vasoactive treatment, oxygenation, restrictive blood transfusion (haemoglobin (Hb) <7 g/dl), hourly monitoring of vital signs and neurological status) and finally, the performance of EGDE and the Rockall and Forrest scores.
Statistical Analysis
Data was analysed using Statistical Package for Social Sciences (SSPS Inc, Chicago, Illinois, USA) version 23.0. Means ± standard deviation was used for quantitative variables; Categorical data was expressed as numbers and proportions. A p value of less than 0.05 was considered statistically significant.
Results
During the retrospective period, 506 patients (prevalence of acute UGIB in the services 5.6%) were included of which 361 men (71.3% and 145 women (28.7 %), given a 2.5 sex ratio. The mean age was 49.9+/- 8 years (maximum 14-96 years) and the peak of bleeding was in the 55-65-year age group. Haematemesis was the initial complaint in 350 patients (69.1%), non-steroidal antiinflammatory drugs (NSAIDs) constituted the most important risk factor in 297 patients (43.6%), in 78 (15.4%). This was a second episode. On admission, clinical parameters relevant to severity were systolic BP <100 mmHg in 122 patients (39.8%); HR >100 beats/ minutes in 435 (85.9%) and RR >20 cycles/minute in 435 (85.9%). Hb was <7g/dl in 359 patients (83.4%). EGDE was performed in 203 patients (40.2%), the major causes of bleeding were: portal hypertension lesions in 111 patients (44.7%) followed by peptic ulcers in 108 (43.5%). Treatment was mainly medical. However, 94 patients (84.7%) with portal hypertension lesions received endoscopic treatment, mainly by injection of sclerosing agent (69.1%), as well as 13 patients (1.2%) with peptic ulcers, mainly isolated injection of dilute adrenaline (1: 10,000) in 11 (84.6%). A total of 75 patients (14.8%) died during hospitalization (Table 2).
The second part concerned the assessment of care offered to 74 patients admitted for acute UGIB (mean age 55 years; sex ratio 2.1). For the recognition of bleeding, digital rectal examination was performed in 43 patients (58.1%) and no patient received nasogastric tube. Regarding the assessment of severity by clinical criteria, BP was taken in 73 patients (98.6%), HR in 61 (82.4%), and RR in 17 (23%), no patient had prognostic scores in the record, including the Glasgow-Blatchford score. Only 17 patients (23%) had SPO2 measurements. Regarding intensive care measures, only 10 patients (13.5%) received a double peripheral venous line, the majority of which was a small-bore venous line. Twenty patients (27%) were filled with crystalloids; restrictive blood transfusion was performed in 24 out of 27 patients (88.9%) with Hb < 7 g / dl. Only 9 patients (12.2%) received nasal oxygen therapy. EGDE was performed in 43 patients (60.6%), all beyond 24 hours after admission and none had a prognostic score after endoscopy (Forrest or Rockall).
Discussion
The study showed that acute UGIB is an emergency with exceptional severity in our environment, as mortality is very high at around 15%. In this study, it was found that acute UGIB affected two and a half times more men than women with a mean age of about 50 years. This is the case in studies conducted in Mali (sex ratio 2.78; mean age 47.45 years), and in Côte d’Ivoire (sex ratio 3.38; mean age 47 years) [8,12]. Indeed, in the sub-Saharan African region, the occurrence of acute UGIB often involves relatively young patients. This can be explained by the fact that the causes of bleeding are often dominated by portal hypertension lesions, especially in young patients, as reported in Mali in a rural area [8]. As opposed to sub-Saharan Africa, in the West, the age of onset of acute UGIB is higher than 70 years due to the use of NSAIDs in the elderly population. Of chronic NSAID users, 25% develop an ulcer, of which 2-4% are complicated by bleeding [2,7,13,14]. The male predominance is universal, and reverses in the West after the age of 80 years due to the higher life expectancy in the female population [2,4,6-9, 11,13,14].
As in several studies reported in literature, hematemesis was the most common initial clinical presentation [2,6,7,15,16]. This initial clinical presentation can be explained by the different lesions found on endoscopy. In fact, portal hypertension lesions, led by oesophageal varices, were the most frequent, alongside peptic ulcers. The frequency of the various aetiologies varies from one region to another [5,6,8]. Thus, in the sub-Saharan African region, several studies report very high frequencies of portal hypertension lesions. This is the case of the study by Diarra et al. in Mali in 2007 [8]. The authors reported a frequency of 55.2% in favour of ruptured oesophageal varices, far ahead of peptic ulcers which represented 16%. The frequency of portal hypertension lesions is also high in Burundi (28.2%) [16] and Gabon (29.5%) [17]. These various countries have liver diseases related to chronic HBV infection in common. Indeed, sub-Saharan African countries are located in a zone of high endemicity according to the World Health Organisation (WHO), i.e. the prevalence of hepatitis B is 8-20% of the general population [10]. Cirrhosis, which causes portal hypertension, is often the result of chronic HBV infection acquired at birth or in early childhood [18]. The annual incidence of varicose veins is approximately 5% [19]. UGIB from ruptured esophageal varices accounts for 70% of gastrointestinal bleeding in cirrhosis, with an estimated overall 2-year bleeding risk of 20% [19]. The aetiological approach to acute UGIB in high- and intermediate-endemic areas where the majority (80%) of the world population lives should therefore consider this high frequency of portal hypertension lesions and bleeding complications.
Regarding the severity of the bleeding, more than 85% of patients were initially unstable with clinical and laboratory signs of severity, despite the absence of Glasgow-Blatchford and Rockall scores in their records. This initial haemodynamic instability can be explained, on the one hand, by the causes of bleeding, in particular the rupture of oesogastric varices, which are exceptionally serious, but also, on the other hand, by the late arrival in hospital structures due to distance, cultural considerations or difficulties of mobility in our country.
Treatment was essentially medical. PPI treatment was most often initiated on admission, even if this treatment did not always fully comply with current recommendations in Europe and Asia [2,7,20,21]. Contrarily, in cases of suspected acute UGIB related to rupture oesogastric varices, vasoactive therapy to reduce portal blood flow was never initiated on admission, in line with international recommendations, including those adapted by the European Society of Gastrointestinal Endoscopy to be applicable to resource-limited settings, including some African countries [2,7,22-24]. Patients with bleeding peptic ulcers have rarely benefited from endoscopic haemostasis, unlike those with portal hypertension lesions. Late arrival at hospital would explain why in sub-Saharan Africa Forrest scores IIc and III, i.e. pigmented stain or clean base of the ulcer, are most frequently found [25]. For the Forrest classification guiding the choice of endoscopic treatment modality for ulcers, there is no endoscopic treatment for these scores [2,3,7,26]. The practice of injecting adrenaline alone instead of combined adrenaline and bipolar coagulation or endoclips was inappropriate. This could be explained by factors such as excessive procedure costs, insufficient training of practitioners and limited logistic equipment.
Read More About Lupine Publishers Journal of Gastroenterology and Hepatology Please Click on Below Link: https://currenttrendsingastroenterology.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.