Lupine Publishers| Journal of Cardiology Research & Reports
Abstract
Heart Failure is a worldwide burden. The prevalence, incidence, mortality and morbidity rates reported show geographic variations, depending on the different aetiologies and clinical characteristics observed among patients with this complex syndrome. In this review we focus on the Afro Caribbean population with Heart Failure providing data review about the Heart Failure etiology based in previous Clinical Trials In addition we provide suggestions based in these Trials and our recent observational clinical studies that might be useful to improve our current Heart Failure Guideline-Directed Medical Therapy . Finally we highlight the need for more regional research.
Keywords: Caribbean region, Heart failure, Etiology, Management
Abbrevations: CHF: Congestive Heart failure; HF: Heart Failure; MI: Myocardial Infarction; SHF: Systolic Heart Failure; HT: Hypertension; DM: Diabetes Mellitus; HFNEF: Heart Failure with a Normal Ejection Fraction; DCM: Dilated Cardiomyopathy; NIDCM: Non-Ischemic Dilated Cardiomyopathy; IDCM: Ischemic Dilated Cardiomyopathy; LVSD: Left Ventricle Systolic Dysfunction; HFmrEF: Heart Failure with mid-range Ejection Fraction; HFrEF: Failure with Reduced Ejection Fraction; ARNI: Angiotens in Receptor Neprilysin Inhibitor
Introduction
There is no doubt that Heart Failure is a complex syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood [1], moreover, Heart Failure is a disease in which there are striking population differences in almost every aspect of the disease. It has been recognized that the cause of Heart Failure is predominantly ischemic disease in nonblack but is related primarily to Hypertension in Blacks [2], accordingly, this statements should be confirmed in Afro-Caribbean patients because population differences exist that may be attributable to differences in social factors, genetics, environment , lifestyle, comorbidities, and complex interactions among this factors [3].
Heart failure research data in African American: can also them be applied in afro Caribbean patients?
The majority of the data on Heart Failure in African descendant has been done in African American population and that research should be validated in the Caribbean Region. The U.S. Office of Management and Budget [4] defines “Black” of “African American” as having origins in any of the Black racial groups of Africa. The term African Caribbean/Afro-Caribbean when used in Europe usually refers to people with African ancestral origins who migrated via the Caribbean islands [5]. The majority of Jamaicans (92.1%) identify as black [6] however there are other ethnic groups [7]: Mixed (6.1%), Asian (0.8%), others (0.4%). Much of Jamaica’s black population is of African or partially African descent with many being able to trace their origins to West Africa and the term African Caribbean must be restricted to an African descent person originating from the Caribbean. Although it seems reasonable to think in terms of African Descendant Data the Heart Failure clinical studies in African American should be validated in the Caribbean Region.
Disparities Between White and Black: Studies In African American Population
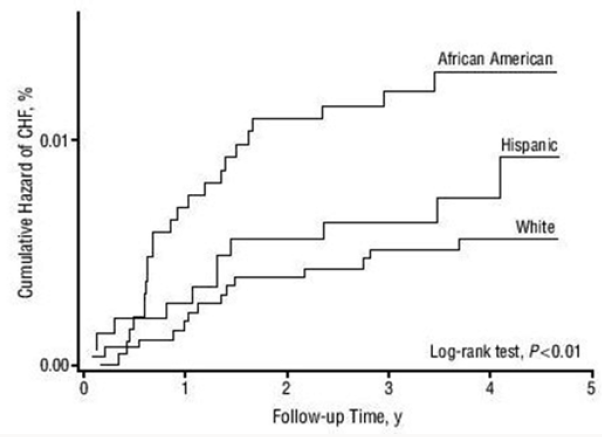
Recent research continues suggesting disparities between white and black populations: In a Random Cohort of 2,188 participants from The Reasons for Geographic and Racial Differences in Stroke Project - REGARDS-[8] without prevalent cardiovascular disease studied by race was showed that Plasma N-terminal pro b-type natriuretic peptide (NTproBNP ) levels are significantly lower in blacks as compared to whites however the contribution of endogenous suppression of Natriuretic Peptide system on cardiovascular disease in blacks remains to be established On the other hand , in relation with the etiology of patients with Heart Failure, when defined as a prior documented myocardial infarction or known epicardial coronary artery disease, ischemic heart disease appears to be present in just 35% of African- American patients and the exact mix of hypertensive heart disease and idiopathic dilated cardiomyopathy (as well as the influence of alcoholic cardiomyopathy) is not discernible from published data. Therefore, the contribution of hypertensive heart disease as the sole explanation of Left Ventricle dysfunction is likely to be between the 30% range reported in the SOLVD registry or the>50% incidence suspected in recently reported β-blocker trials [9] (Figure 1). Moreover in the Multi-Ethnic Study of Atherosclerosis --MESA-[10] , a cohort study of 6814 participants of 4 ethnicities (African American :27.8%) , African Americans had the highest incidence rate of Congestive Heart failure (CHF) and showed that the mechanisms of CHF also differed by ethnicity namely an interim myocardial infarction had the least influence among African Americans (Figure 2).
Figure 1: Heart Failure in African Americans: Incidence of Coronary Artery Disease. Pooled Data from major Trials in Heart Failure reporting probable cause of Left Ventricle Systolic Dysfunction. US Carv= =US Carvelidol Heart failure Trials Program; BEST=Beta Blocker Evaluation of Survival Trial; AA=African American; Non-AA=Non African American [9].
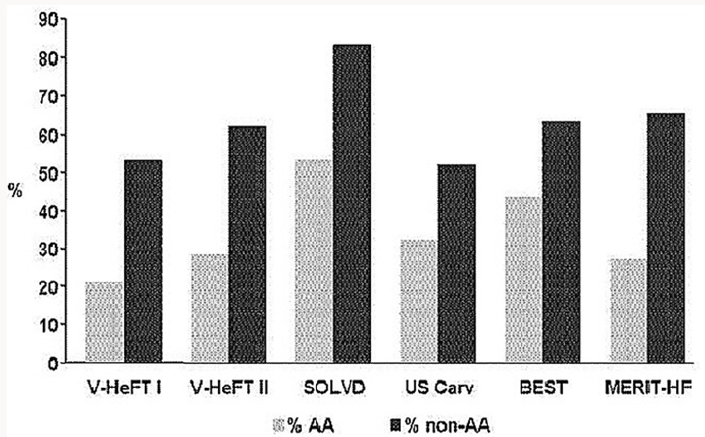
Figure 2: Nelson-Aalen Plots of Cumulative Hazards for Congestive Heart Failure (CHF) among Multi-Ethnic Study of Atherosclerosis Study participants without an interim Myocardial Infarction [10].
That is , as the Time course and pattern of development of heart failure (HF) can be primarily caused by myocardial infarction (MI), with pronounced remodeling and shape change leading to systolic heart failure (SHF) or HF primarily caused by hypertension (HT), with or without diabetes mellitus (DM), leading to heart failure with a normal ejection fraction (HFNEF) however both, patients with a history of MI and patients with HT may experience periods of HFNEF and finally Systolic heart failure (SHF) with a reduced ejection fraction: HFrEF [11] .More evidence about the Primary Cause of Heart Failure in African American can be also analyzed from the Baseline Characteristics of the African-American Heart Failure Trial [12] in which about 1000 patients showed a history of Ischemic Heart Disease in just 23% and also in the recent Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGMHF) Sub study [13] in which the Black participants (N=428) showed a history of Myocardial Infarction in just 17.3 % vs 48.3 % in the White participants (N=5544) , strengthening the Heart Failure mechanism with less influence of an interim of a myocardial infarction. From the few studies among Afro Caribbean population with Heart Failure is worth mentioning the study of Afro-Caribbean heart Failure in the United Kingdom [14]: compared with the white population, Heart Failure in Afro Caribbean Patients (n=211) was mostly associated with Non Ischemic Cardiomyopathy (87vs 59%), Dilated Cardiomyopathy (27.5 vs 10.8%) and Hypertensive Cardiomyopathy (12.3 vs 2.2%) and even more interesting is the fact that Cardiac Amyloidosis was confirmed in 11.4 vs 1.6% .
Heart failure in african-americans
As suggested for previous Clinical Trials Experience, Heart Failure Etiology [15] in African-Americans-AA:
a) Is much more associated with Non Ischemic etiology of Left Ventricular Dysfunction (LVD).
b) Hypertension is considered the putative disease process but dilated cardiomyopathies and Diabetes-related diseases are common.
c) Coronary Artery Disease remains a cause of LVD but is less common in AA than in whites.
Why African Americans, and extensively Afro-Caribbean, have more Heart Failure?
It has been proposed [16] the following mechanisms:
a) The impact of Modifiable Risk Factors.
b) Neuro hormonal imbalances and endothelial dysfunction.
c) Genetic Polymorphisms and
d) Socioeconomic Factors and Quality of Care.
It is clear that Hypertension remains as the most important risk factor: A Prevalence estimates for traditional CVD risk factors in Jamaicans showed [17]: hypertension, 25%; diabetes, 8%; hypercholesterolemia, 12%; obesity, 25%; smoking 15%. In addition, 35% of Jamaicans had pre hypertension, 3% had impaired fasting glucose and 27% were overweight. A higher proportion of women had diabetes, obesity and hypercholesterolemia while the prevalence of pre hypertension and cigarette smoking was higher in men. In the other hand, some race-specific differences in endothelial function and predisposition of AA to vascular diseases are [18]: (a) increased oxidative stress (b) decreased Nitrite Oxide availability (c) Exaggerated vasoconstrictor response and (d) attenuated responsiveness to Vasodilators and Nitric Oxide. In addition, Genetic Polymorphisms associated with the risk of Heart failure in AA has been considered [16] : (a) Beta 1 Adrenergic Receptor (b) Alpha 2c Adrenergic Receptor (c ) Aldosterone Synthase (d) G Protein (e) Transforming G Grow Factor Beta (f) Nitric Oxide Synthase (g) Transthyretin. This has been recently evaluated for Dungu [14]: In a comparison with white patients, the author found ATTR V122l and Cardiac Amyloidosis all types in 8.5 % vs 0.3 % and 11.4% vs 1.6 % respectively of Afro-Caribbean vs. White patients with Heart Failure living in the United Kingdom.
Clinical studies in afro-caribbean patients with heart failure living in jamaica
The available data of Afro Caribbean Heart Failure, including studies in Jamaica, is scarce. Tulloch Reid [19] brought the attention to cases with unexplained Dilated Cardiomyopathy and reported the association of HTLV-1 seropositivity and Unexplained Dilated Cardiomyopathy (DCM) in Jamaican patients. This author also reported the experience of 26 cases (45±11 years-old) with unexplained dilated cardiomyopathy at Kingston Public Hospital (personal communication). Lalljie [20] reported the experience in 100 Jamaican with heart failure patients: 49% had echocardiograms, of these 39% had ejection fractions (EF)>40%, 34 % had EF 21-40 % and 27% had EF<20%. Hypertensive heart disease was found in 54%, hypertensive cardiomyopathy in 14 % and ischemic heart disease just in 26 %. Accordingly and knowing that the majority of the data on Heart Failure in African descendant has been done in African American population and that these studies had to be validated in the Caribbean Region we planned some observational studies [21-23] in order to know:
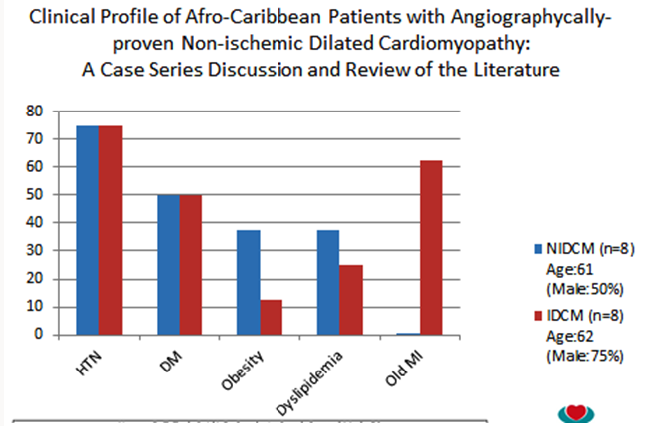
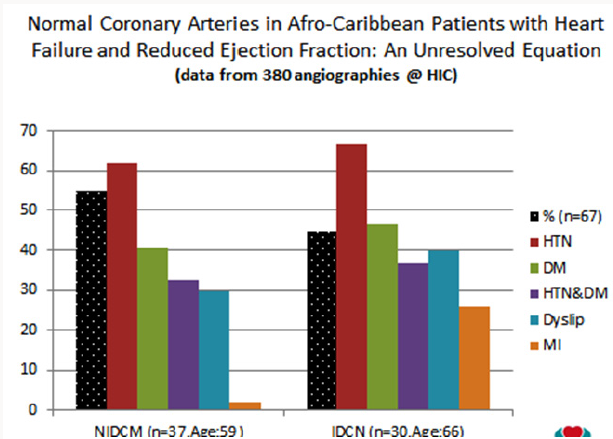
a) The cardiovascular risk profile of patients with, angiographycally proven, Non-Ischemic Dilated Cardiomyopathy (NIDCM) vs Ischemic Dilated Cardiomyopathy (IDCM) (Figure 3).
Figure 3 : The presence or the absence of the most important traditional cardiovascular factors (Hypertension=HTN and Diabetes-DM), which have been described as strongly correlated with coronary artery disease, are not necessarily predictive of angiographycally-proven Non-Ischemic Dilated Cardiomyopathy (NIDCM) in an Afro Caribbean population with HFrEF [21].
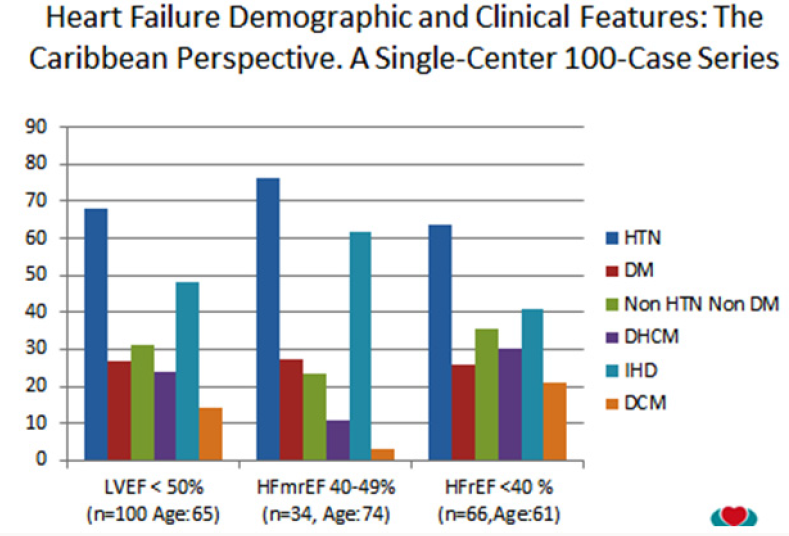
b) The demographic and clinical features of patients with left ventricle systolic dysfunction (LVSD) and differences between Heart Failure with mid-range Ejection Fraction (HFmrEF) and Heart Failure with Reduced Ejection Fraction (HFrEF) (Figure 4).
Figure 4 : The presence or the absence of the most important traditional cardiovascular factors (Hypertension=HTN and Diabetes-DM), which have been described as strongly correlated with coronary artery disease, are not necessarily predictive of angiographycally-proven Non-Ischemic Dilated Cardiomyopathy (NIDCM) in an Afro Caribbean population with HFrEF [21].
c) The proportion and clinical features of patients with angiographycally proven Ischemic vs Non Ischemic Heart Failure with Reduced Ejection Fraction (HFrEF) from our Coronary Angiographies database (Figure 5).
Figure 5 : From a total of 380 patient’s angiographycally evaluated during the study period, 67 patients were included in the analysis. The prevalence (%) of patients with NIDCM was 55%. With the exception of age (59 vs 65, p<0.03) and confirmed myocardial infarction-MI (2 vs 25%, p<0.04) there were no significant differences (p<0.05) in the prevalence of CAD risk factors suggesting that among Afro-Caribbean patients with HFrEF, despite that both groups of patients were exposed to similar CAD risk factors, angiographycally proven NIDCM is more frequent that IDCM. This underlines the hypothesis that other factors may play an important role in the etiology of the Afro Caribbean Heart Failure [23].
Lessons From the Clinical Studies on Afro Caribbean Patients with Heart Failure Living in Jamaica
From a broad perspective, these studies are suggesting that:
a) Although both groups (NIDCM vs IDCM) has been exposed over their lifetime to the same strong risk factors for CAD, they potentially and can develop the same outcome (DCM) but one group with angiographycally normal epicardial coronary arteries and the other with angiographycally abnormal coronary arteries.
b) Hypertension and Diabetes are the most important risk factors associated with Dilated Cardiomyopathy in this Afro Caribbean population.
c) Afro-Caribbean patients with heart failure and are mainly hypertensive with or without diabetes and grossly half of them develop LVSD due to non-ischemic causes.
d) They demonstrate a distinct etiological but similar clinical profile when they are classified in the category of HFmrEF and HFrEF
e) Among Afro-Caribbean patients with HFrEF, angiography ally proven NIDCM is more frequent (55vs.45%) that IDCM suggesting that despite both groups of patient’s exposure to the similar CAD risk factors, other factors play an important role in etiology of the left ventricle failure.
Understanding Afro Caribbean Heart Failure to Improve the Management Practices
According with the 2013 ACC/HFA Guidelines [1] the magnitude of benefit for Reduction in Mortality and Reduction in HF Hospitalizations demonstrated in RCTs is ,respectively, as follows: a) ACE Inhibitor or ARB: 17% and 31% b) Beta Blockers: 34% and 41% c) Aldosterone Antagonist: 30% and 35% and d) Hydralazine/ Nitrate (HYD/ISDN): 43% and 33%, accordingly the Pharmacologic treatment recommendation for persistently symptomatic African American patients with Stage C HFrEF, class III-IV, in order to reduce morbidity and mortality, and in addition to ACE Inhibitor, or ARB and in conjunction with Beta Blocker is Hydralazine/Nitrates (Class I, LOE A). Moreover, the 2017 ACC/AHA Guidelines Update [24] has recommended for patients with chronic HFrEF, to reduce morbidity and mortality the Angiotens in Receptor Neprilysin Inhibitor (ARNI) in conjunction with Beta Blocker (Class I, LOE B-R) and for patients with chronic symptomatic HFrEF, NYHA class II-III, who tolerate an ACE Inhibitor or ARB: the ARNI, to replace an ACE Inhibitor or ARB (Class I, LOE B-R) More understanding about the population of African Americans has been mentioned in the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure with Reduced Ejection Fraction [25] which has stated that in African Americans Sacubitril/Valsartan and Ivabradine were tested in populations with few African Americans receiving HYD/ ISDN. Thus, for this population, there are no data for the efficacy or safety of ARNI in patients with an indication for HYD/ISDN.
Moreover, both HYD/ISDN and ARNI purportedly act via upregulation of cGMP pathways, which may increase the risk of hypotension. Additionally, the risk of angioedema with ACEI and ARNI is particularly high in African-American patients (0.5% with ACEI and 2.4% with ARNI); this risk, however, should not preclude initiation of these agents absent a documented history of angioedema. Two options would exist: A. Establish Guideline- Directed Medical Therapy (GDMT) with ACEI/ARB, beta blocker, and an aldosterone antagonist, then switch to ARNI; if stable, follow with HYD/ISDN if patient has persistent class III to IV symptoms with careful blood pressure monitoring or B. Establish GDMT with ACEI/ARB, beta blocker, and an aldosterone antagonist and then proceed with HYD/ISDN if persistent class III to IV symptoms; if stable, follow with ARNI substitution for ACEI/ARB with careful blood pressure monitoring. In the absence of randomized controlled data, it is reasonable to treat an African-American patient using either approach. However, the risk for hypotension with either strategy is uncertain. The treatment decision should be determined after an informed shared decision-making discussion with the patient, indicating the uncertainty of benefit.HYD/ISDN is available as a fixed-dose combination or as individual medications. The ACC/ AHA/HFSA guideline considers either as acceptable in this context.
Conclusion
Heart Failure is a complex syndrome. The prevalence, incidence, mortality and morbidity rates reported show geographic variations, depending on the different aetiologies and clinical characteristics observed among patients. In this review we focus on the Afro Caribbean population with Heart Failure providing data review about the Heart Failure etiology based in previous Clinical Trials In addition we provide suggestions based in these Trials and our regional clinical studies that might be useful to improve our current Heart Failure Guideline-Directed Medical Therapy There is a need to understanding more the epidemiology and mechanisms of Afro Caribbean Heart Failure in order to improve the current management practices from a Caribbean perspective. At this time there are no studies on the use of ARNIs in the unique Afro Caribbean population, accordingly clinical experience studies with regards to the tolerance and safety of sacubitril/valsartan to prospectively identify adverse events and discontinuation for adverse events in patients with HFrEF are required.
Read More About Lupine Publishers Journal of Cardiology Research & Reports Please Click on Below Link: https://lupine-publishers-cardiovascular.blogspot.com/

No comments:
Post a Comment
Note: only a member of this blog may post a comment.