Open Access Journal of Complementary & Alternative Medicine | lupine Publishers
Abstract
Introduction
Who is at risk?
Awareness of risk factors can help to take steps to reduce bone mineral loss. Fixed risk factors like disorders and medications can weaken bone and affect balance [2]. Fixed risk factors include increasing age, female gender, family history of osteoporosis, ethnicity, menopause, hysterectomy, rheumatoid arthritis, hypogonadism in men etc. Most modifiable risk factors like alcohol, smoking, low body mass index, poor nutrition, vitamin D deficiency, eating disorders, physical inactivity also can directly impact bone biology and result in a decrease in bone mineral density (BMD).Preventing osteoporosis
It is now known that osteoporosis is a preventable and treatable disease and not a normal part of ageing [3]. Although genetic factors play a significant role in determining whether an individual is at heightened risk of osteoporosis, lifestyle factors such as diet and physical activity also influence bone development in youth and the rate of bone loss later in life. After mid-20s, bone thinning is a natural process and cannot be completely stopped. The thicker the bones, the less likely they are to become thin enough to break. Young women in particular need to be aware of their osteoporosis risk and take steps to slow its progress and prevent fractures. Optimal bone growth and development in youth is vital in the prevention of osteoporosis as it is an important determinant of the risk of osteoporotic fracture during later life. It is estimated a 10% increase of peak bone mass in children reduces the risk of an osteoporotic fracture during adult life by 50% [4]. Once peak bone mass has been reached, it is maintained by a process called remodeling. This is a continuous process in which old bone is removed and new bone is created. The renewal of bone is responsible for bone strength throughout life. Factors that cause a higher rate of bone remodeling will ultimately lead to a more rapid loss of bone mass and high risk of fractures. Adequate calcium levels are crucial for bone health and muscle performance, which are closely associated with balance and fall risk [5]. Vitamin D plays a major role to maintain serum calcium levels through enhancement of small-intestine absorption [6]. Sunlight exposure, fortified foods, egg yolks, saltwater fish, liver, are rich sources of Vitamin D. Due to increasingly indoor lifestyles, young people often don’t get enough vitamin D. Parents should encourage children spend more time participating in sports and outdoor physical activity and less screen time in front of computers or televisions to maintain a healthy level of this key vitamin.How is osteoporosis diagnosed?
Though traditional X-rays cannot measure bone density, they can identify spine fractures. Dual energy X-ray absorptiometry (DEXA) is the best technique for diagnosis and monitoring therapy. It is a low radiation X-ray used to measure spine and hip bone density and can also measure bone density of the whole skeleton. Other methods for diagnosing osteoporosis like Bone Turnover Markers (BTM) and radiological assessments have been used extensively in clinical trials and epidemiological studies.Medical Management
Regular exercise is essential
Regular exercise helps decreasing the risk of falls, probably because balance is improved, and muscle strength is increased. Build up slowly and aim to gradually increase the repetitions of each exercise over time. It is important to avoid exercises that can injure already weakened bones. In patients over 40 and those with heart disease, obesity, diabetes mellitus, and high blood pressure, exercise should be prescribed and monitored by physicians. Extreme levels of exercise like lifting heavy weights and forward bending may not be healthy for the bones. Exercises to correct postural deformities like Dowager’s hump should be incorporated in therapy.Weight-bearing exercises
Several studies demonstrate the health benefits of exercise, including reduced risk of falls and fractures. Weight-bearing and muscle-strengthening exercises are ideal for osteoporosis prevention because it improves agility, posture, balance, and strength to prevent falls [5]. A statistically significant effect of exercise on BMD was reported by a systematic review investigating whether exercise could prevent bone loss and fractures in postmenopausal women [9]. It was found that high-force exercise involving lower limbs was the most effective exercise for femur neck BMD. Brisk walking is highly recommended, and patients can adapt their speed to the current fitness level. Sit-to-stand, Mini-squats, Calf raises, Wall press-up, Push-ups are good examples of exercises that patients can perform at home. Low-impact weight-bearing exercises like aerobics, using stair-step machines, fast walking on a treadmill are advised if high force exercises are contraindicated.Muscle-strengthening exercises
Numerous studies have shown that strength training can play a role in slowing bone loss, and several show it can even build bone [10,11]. This is tremendously useful to help offset age-related declines in bone mass. Activities that put stress on bones can nudge bone-forming cells into action. Body weight exercises like squats, sit to stand; rising up on your toes can be performed at home. Lifting weights, using elastic exercise bands and using weight machines use muscle strength, where the action of the tendons pulling on the bones boosts bone strength. High-impact weight-bearing exercises help build bones and keep them strong. Cycling and swimming do not cause positive effects on BMD; thus, these are not the most suitable exercises for prevention and treatment of osteoporosis [12]. Swimming is neither a weight-bearing exercise nor a strengthtraining exercise. This means that if you are trying to prevent or fight osteoporosis, swimming should not be the only workout that you do.Diet is Important
Preventing falls
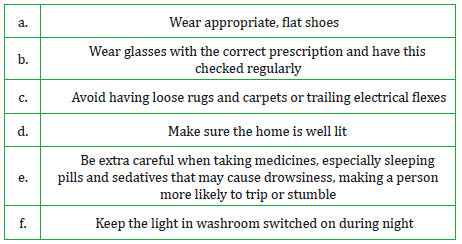
Fall prevention helps prevent osteoporosis-related morbidity. Interventions include vision and hearing correction, removing trip or fall hazards, evaluating suspected neurologic problems, avoiding medications that cause imbalance, and advising hip pad protectors for those with significant risk. A person with osteoporosis is especially at risk of breaking bones from falling because the bones are so much weaker than normal healthy bones. Certain steps that can make a house safer for someone with osteoporosis is shown in Table 1.The most effective treatment is provided by multidisciplinary approach involving physical therapist, psychologist, and nutritionist for consultation. Clinicians should consider risk-assessment to estimate absolute fracture risk and appropriate pharmacologic agents to prevent osteoporosis are to be prescribed [16].
Life style factors
Maintaining healthy habits can also reduce the risk or severity of osteoporosis. Smoking is an independent risk factor for osteoporosis as it reduces the amount of estrogen the body produces, and alcohol hinders calcium absorption [17]. It is also critical to maintain a healthy body weight. Nutrition is a modifiable pathogenic factor for osteoporosis. A holistic approach to bone health combining nutrition, physical activity and fall prevention is the key. Impactful public health education initiatives can create awareness about osteoporosis. Social media like Facebook groups and Twitter that provide a number of tools and resources as well as a forum for people to discuss osteoporosis shall be considered. Community programs with non-profit organizations reinforced at the local level can extend the program’s reach and messages.Conclusion
For more Lupine Publishers Open Access Journals Please visit our website:
https://lupinepublishersgroup.com/
For more Open Access Journal of Complementary & Alternative Medicine Please Click Here:
https://lupinepublishers.com/complementary-alternative-medicine-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers

No comments:
Post a Comment
Note: only a member of this blog may post a comment.